PCOS, anovulatory cycles and hyperinsulinemia – PCOS 9

Anovulatory cycles
Anovulatory cycles are menstrual cycles where no ovulation occurs. 70% of anovulatory infertility is related to PCOS.During follicular arrest, no dominant follicle grows large enough to ovulate. Without a mature egg, conception cannot occur, leading to the devastating realization that one cannot have a baby.
During normal menstruation, progesterone is produced after ovulation by the remnant of the dominant follicle. Without ovulation, this does not occur and there is too little progesterone leading to heavy periods and irregularity. This leads clinically to the irregular cycles found in PCOS. Almost all women will experience some anovulatory cycles in their lifetimes, especially during puberty and menopause.
However, the underlying cause of the anovulation is the excessive insulin and testosterone once again. Since testosterone is mostly overproduced due to high insulin, the singular, most responsible culprit for anovulatory cycles is likely high insulin. Weight loss and metformin both lower plasma T and improve ovulatory rates, and is the reason metformin is widely used in this disease. Indeed, all known treatments to reduce insulin, including weight loss, bariatric surgery, the drugs somatostatin and metformin significantly improve ovulatory function and symptoms of PCOS. Interestingly, patients with type 1 diabetes using high doses of injected insulin also have an increased risk of PCOS.
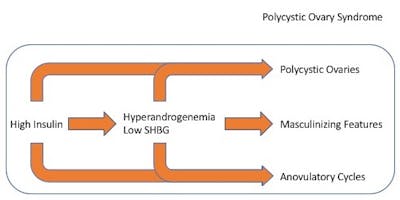
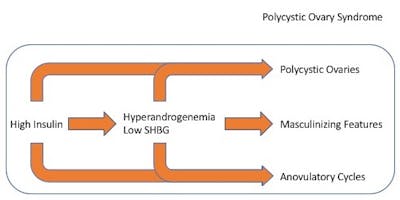
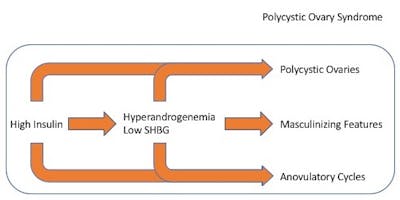
The three defining features of PCOS include polycystic ovaries, anovulatory cycles, and masculine features. All three symptoms reflect the same pathophysiology – too much testosterone, ultimately caused by too much insulin.
Simply put – too much insulin causes PCOS.
Insulin resistance
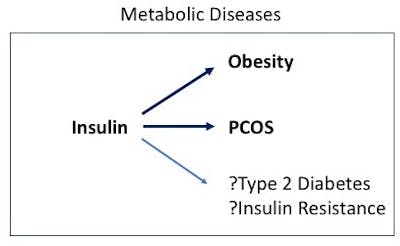
PCOS is best understood as a disease of hyperinsulinemia. This explains the close connection between obesity and PCOS –they can both be manifestations of underlying hyperinsulinemia. They do not always occur together but are closely associated. But what is causing the high insulin levels?
Dietary factors, such as excessive calories, sugar and refined carbohydrates, are certainly important, but they are not the only factor causing high insulin. The other major factor that increases insulin is the presence of a condition known as insulin resistance.
Recall that insulin is a hormone that moves glucose from the blood inside the cells. In the state of ‘insulin resistance’, the normal insulin levels are not able to move glucose inside. The body responds by ramping up insulin levels to force the blood glucose into the cells. Thus, insulin resistance is a key factor in keeping insulin levels high, even without any change in the diet.
PCOS is highly associated with both insulin resistance and hyperinsulinemia. Insulin sensitivity is decreased on average 30-40% in women with PCOS, a degree similar to that seen in type 2 diabetes. Obesity itself is highly linked to insulin resistance, but it is also present in normal weight adolescents with PCOS. Even independent of obesity, insulin resistance is diagnosed in 75% of lean women with PCOS. In overweight women with PCOS, this proportion increases to a massive 95%. Essentially, all overweight women with PCOS have evidence of insulin resistance. In addition, normal weight girls with PCOS had evidence of more fatty liver than those without PCOS, another disease associated with insulin resistance. Increased insulin resistance is the essential feature of type 2 diabetes.
So, insulin resistance causes high insulin levels which will contribute to PCOS. But what causes this insulin resistant state in the first place? It turns out it can be the high insulin levels itself. We’ve discussed this previously in the entire series on Diabetes as well as in my book, The Diabetes Code.
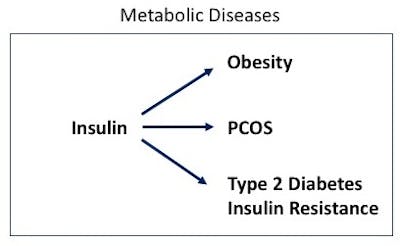
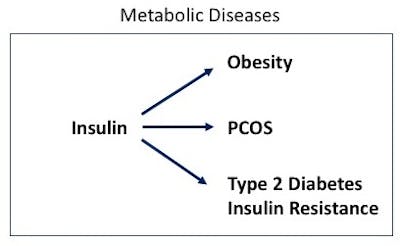
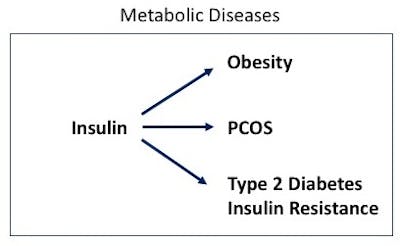
So, PCOS is really just another manifestation of metabolic disease, all of which are caused by too much insulin – hyperinsulinemia. This is crucial knowledge, because if the root cause of PCOS (and obesity and type 2 diabetes) is too much insulin, then the solution becomes fairly obvious – lower insulin. How to do that? The solution is certainly not drilling holes into the ovary. The solution is largely dietary. Low-carbohydrate diets and fasting are two effective option..
Also published on idmprogram.com.
Earlier
PCOS and hyperinsulinemia – PCOS 8
PCOS and hyperandrogenism – PCOS 7
PCOS and associated conditions – PCOS 6
The difficulties of diagnosing PCOS – PCOS 4
Dr. Fung’s top posts
Type 2 diabetes
Weight loss
Keto
Intermittent fasting
More with Dr. Fung
Dr. Fung has his own blog at idmprogram.com. He is also active on Twitter.
Dr. Fung’s books The Obesity Code, The Complete Guide to Fasting and The Diabetes Code are available on Amazon.