The obesity epidemic

I grew up in Toronto, Canada in the early 1970s. My younger self would have been utterly shocked that today, obesity has become a rising, unstoppable global phenomenon. At that time, there were serious Malthusian fears that the world’s population would soon eclipse the world’s food production and we would face mass starvation. The major environmental concern was global cooling due to the reflection of sunlight off dust particles in the air triggering the dawn of a new Ice Age. I wonder if Time Magazine thought one of the 51 things we should do is to become a penguin…
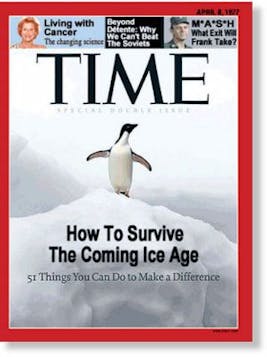
Instead, some 50 years later, we find ourselves facing exactly the opposite problems. Global cooling has long ceased to be a serious concern, but global warming and melting polar ice caps dominate the news. Instead of global hunger and mass starvation, we face an obesity epidemic, unprecedented in human history.
There are many puzzling aspects to this obesity epidemic. First, what caused it? The fact that this epidemic is both global and relatively recent argues against an underlying genetic defect. Exercise as a leisure activity was largely unheard of in the 1970s. People just didn’t sweat with the oldies in that decade. The proliferation of gyms, running clubs, exercise studios and the like were a product of the 1980s. I would struggle with this question for many years. People ate white bread, ice cream and Oreo cookies in the 1970s. Whole wheat pasta and bread didn’t truly exist as foods real people ate. They were doing everything ‘wrong’ but yet there’s little obesity, as you can easily see if you were to look at old photographs from the 1970s.



The lack of interest in nutrition
In the 1990s, I graduated from the University of Toronto and the University of California, Los Angeles as a physician and kidney specialist. And I must confess that I did not have the slightest interest in the treatment of obesity. Not during medical school, residency, specialty training or even during practice. But it wasn’t just me. This was true for just about every physician trained in North America. Medical school taught us virtually nothing about nutrition, and even less about the treatment of obesity. There were hours and hours of lectures dedicated to the proper medications and surgery to prescribe. I was proficient in the use of hundreds of medications. I was proficient in the use of dialysis. I knew all about surgical treatments and indications. But I knew nothing about nutrition and even less about how to lose weight. This is despite the fact that the obesity epidemic was well established, and the epidemic of type 2 diabetes was following just behind, with all its health implications. We didn’t talk enough about diet.
Weight loss was not a matter of looking good in a bikini for the summer swimming season. If only. The excess weight was largely responsible for development of type 2 diabetes and metabolic syndrome, dramatically increasing the risk of heart attacks, stroke, cancer, kidney disease, blindness, amputations, and nerve damage, among other problems. This was not some peripheral topic of medicine. Obesity was at the very heart of everything, and I knew just about nothing.
I entered practice as a kidney specialist in the early 2000s, and the most common cause of kidney failure, by far, was type 2 diabetes. I treated those patients exactly as I had been trained, the only way I knew how. With drugs like insulin and procedures like dialysis.
From experience, I knew that insulin would cause weight gain. Actually, everybody knew insulin caused weight gain. Patients were rightly concerned. “Doctor,” they say, “you’ve always told me to lose weight. But the insulin you gave me makes me gain so much weight. How is this helpful?” For a long time, I didn’t have a good answer for them, because the truth was it wasn’t helpful.
The problem was that my patients were just not getting healthier. I was simply holding their hand as they got worse and worse. I was doing everything I was taught, but it wasn’t doing any good. Gradually, it dawned on me what the problem was.
The root cause of much of the problem was the weight. Obesity caused metabolic syndrome and type 2 diabetes, which caused all the other problems. Yet everything I was taught, almost the entire system of modern medicine, with its pharmacopeia, with its nanotechnology, with all the genetic wizardry was focused myopically on the problems at the end.
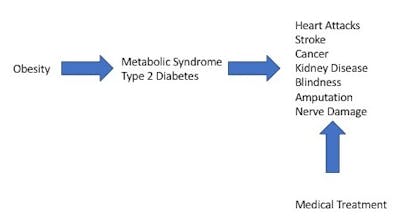
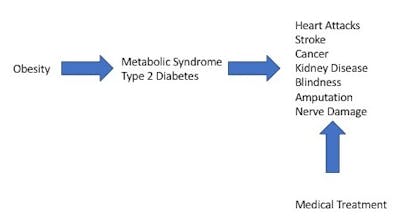
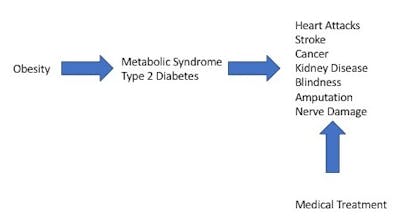
Nobody was treating the root cause. If you treat the kidney disease, patients are still left with obesity, type 2 diabetes and every other complication. This was the way that I, and virtually every other doctor was trained to practice medicine. But it was not working. We needed to treat obesity. We were trying to treat the problems caused by obesity rather than obesity itself.
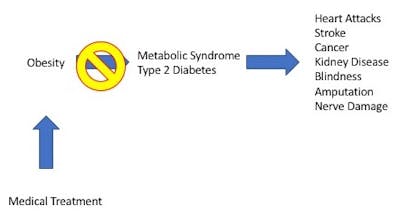
When people lost weight their type 2 diabetes would commonly reverse course. Treating the root cause is the only logical solution. If your car is leaking oil, the solution is not to buy more oil and mops to clean the spilled oil. The logical solution is to find the leak and fix it. As a medical profession, we were guilty of ignoring the leak.
If you could treat the obesity at the beginning, then type 2 diabetes and metabolic syndrome likely would not develop. You couldn’t develop diabetic kidney disease if you didn’t have diabetes. You couldn’t develop diabetic nerve damage if you didn’t’ have diabetes. It seems obvious in retrospect.
How can obesity be treated?
The problem was that I didn’t know how to treat the obesity. Despite having worked more than twenty years in medicine, I found that my own nutritional knowledge was rudimentary, at best. This sparked a decade long odyssey and eventually led me to establish the Intensive Dietary Management (IDM) program and the Toronto Metabolic Clinic.
In thinking seriously about the treatment of obesity, there was one singularly important question to understand. What causes weight gain? What is the root cause? The reason we never think about this crucial question is that we already think we know the answer. We think that eating too many calories causes obesity. If this were true, then the solution to weight loss is simple. Eat fewer calories.
But we’ve done that already. Ad nauseam. For the last 50 years, the most common weight loss ever given out was to cut your calories and exercise more. This is the highly ineffective strategy called ‘Eat Less, Move More’. We’ve added calorie counts to food labels. We have calorie counting books. We have calorie counting apps. We have calorie counters on our exercise machines. We’ve done everything humanly possible to count calories so that we could cut them. Did it work? Did those pounds melt like a snowman in July? No. It sure sounds like it should work. But the empiric evidence, plain as a mole on the tip of your nose, is that it does not work.
From a human physiology standpoint, the entire calorie story collapses like a house of cards. The body does not measure calories because it has no calorie sensors. The body does not respond to ‘calories’. There are no calorie receptors on cell surfaces. It has no ability to know how many calories you are or are not eating. If your body doesn’t count calories, why should you? Calories is purely a unit of energy borrowed from physics. The field of obesity medicine, desperate for some simple measure of food energy, completely ignored human physiology and turned to physics instead.
So, we got the saying ‘A calorie is a calorie’. But that’s not a question I can recall anybody ever asking. Instead, the question is ‘Do all calories of food energy equally lead to weight gain?’, to which the answer is an emphatic no. One hundred calories of kale salad do not have the same effect as one hundred calories of candy. One hundred calories of beans is not equalbto one hundred calories of white bread and jam. But for the last 50 years, we pretended they equally led to obesity
And so I started from the beginning. Unraveling the rotten tapestry of the Calories model to answer that all-important question of the underlying causes of weight gain was the reason I wrote The Obesity Code. Since then, in my Intensive Dietary Management program (www.IDMprogram.com) has treated thousands of patients over the last 5 years. I’ve wondered sometimes about why such a simple concept about using free dietary measures like fasting to treat dietary diseases runs into such obstacles. We can change that. We can reverse the obesity and diabetes epidemic.
Dr. Fung’s top posts
Weight loss
Keto
Intermittent fasting
More with Dr. Fung
Dr. Fung has his own blog at idmprogram.com. He is also active on Twitter.
Dr. Fung’s books The Obesity Code, The Complete Guide to Fasting and The Diabetes Code are available on Amazon.