Cutting calories won’t solve your weight issues – do this instead

Contrary to what most people believe, long-term weight loss is not simply about cutting a few calories here and there. Sure, it sounds like it works, but the bottom line is that for most people it does not. This has been proven in numerous studies and also the countless tears of unsuccessful dieters desperately counting their calories like Ebenezer Scrooge counting his pennies.
We pretend we live in a world where nutrition demands scientifically rigorous proof that prescribed treatments are effective. So, where are the studies that show that cutting calories causes long-term weight loss? After 50 years of desperate, intense research, guess how many studies prove its long-term effectiveness? How about zero? That’s right, Nada. Zilch. Zero.
The only reason we think the ‘caloric reduction as primary’ strategy is effective is because it’s been repeated so often. It’s like Santa Claus. When I was a kid, I thought “So, some random guy is just going to give me presents for no reason?” But repeated often enough, these tales gain an undeserved sheen of truth.



In our bodies, we have the BSW, also called an appestat or obesistat, essentially a thermostat for body fatness. Some people believe we are designed to eat everything in front of our face and now that food is so easily available, we have no choice but to gain weight. This completely ignores normal human physiology.
Instead, we have multiple overlapping powerful satiety mechanisms to stop eating. We have stretch receptors in our stomach to signal when it is too full. We have powerful satiety hormones such as peptide YY and cholecystokinin that stop us from eating. Think about a time you’ve eaten too much at a Chinese buffet. Would you be able to eat two more pork chops, just because they are available and free? Think about those restaurants that will give you a free meal if you can eat 40 oz of steak in 1 hour. Are they going bankrupt anytime soon? No. Because it is really, really hard to keep eating once we’re full. Yet these are the very same pork chops or steak that we hungrily ate just a few minutes ago, prior to the meal.
From an evolutionary standpoint, these satiety mechanisms make a lot of sense. Our body is designed to stay within certain body-fat parameters. If you are too skinny, you will die during the hard times (winter). If you are too fat, you will not be able to catch food, and you might just get eaten yourself. Wild animals almost never become obese to the point of being unable to function normally. Where are the morbidly obese antelope? Caribou? Lions? Tigers? Fish? When food is plentiful, numbers of animals increase. You don’t get a few morbidly obese rats. You get thousands of relatively normal-sized rats.
The body set weight
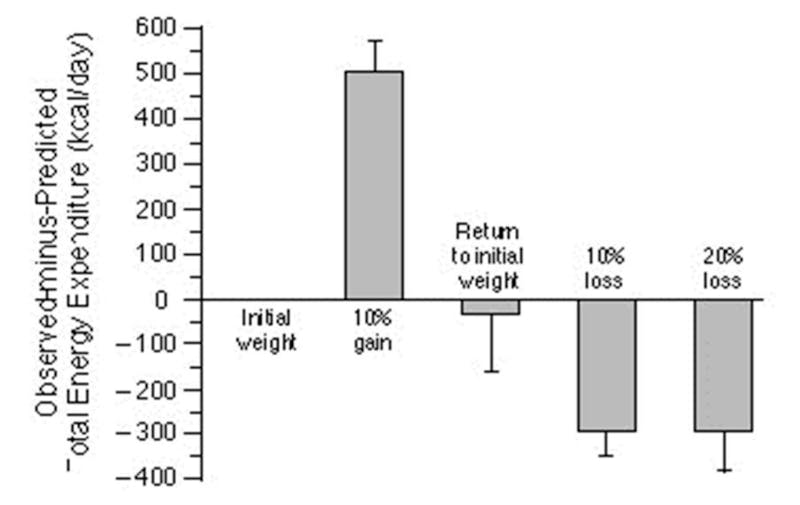
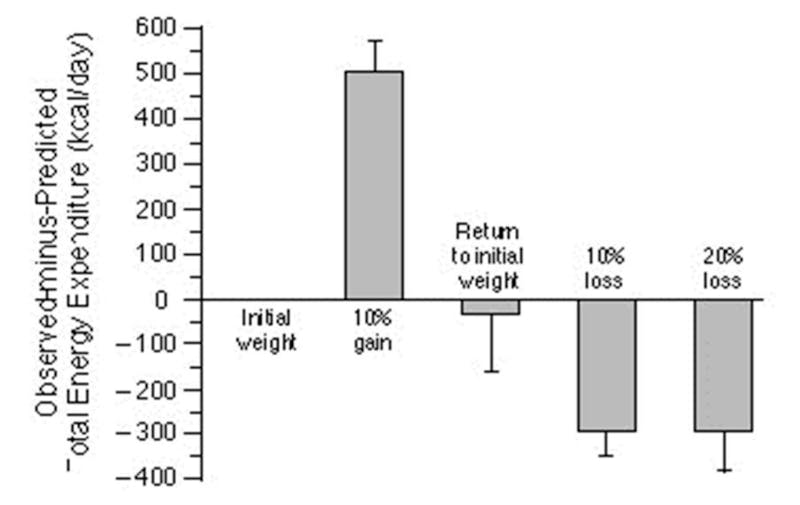
The BSW sets an ideal body fatness that it defends just like our house thermostat. If we are too skinny, we try to gain weight. If we are too fat, we try to lose weight.The clearest experimental demonstration of this was done by Dr. Rudy Leibel in 1995. In this experiment he took volunteers, and overfed them to make them gain 10% more weight. Then he returned them to their regular weight, and then to 10% or 20% weight loss. At each point, he measured the basal metabolic rate (BMR), or how much energy (calories) the body is expending. After 10% weight gain, the body burns about 500 calories more per day compared to baseline. As the body returns to it’s original weight, so does the metabolic rate. After 10% weight loss, the body burns about 300 calories per day less.
The body tries very hard to maintain its BSW in the original position, acting just like our house thermostat. This directly contradicts the Calories In/ Calories Out (CICO) viewpoint that hold that simply eating too many calories causes body fatness without regard to the BSW or satiety hormones or pretty much any other physiologic signaling. If you deliberately overeat, your body tries to burn it off.
‘Calories’ is not a physiologic notion, as we’ve previously discussed. Our body has no ‘calorie’ receptors and does not know how many calories we eat or don’t eat. Over the past several centuries, we’ve decoded many of the human metabolic pathways. Do you see ‘calories’ mentioned ANYWHERE in this complex diagram?
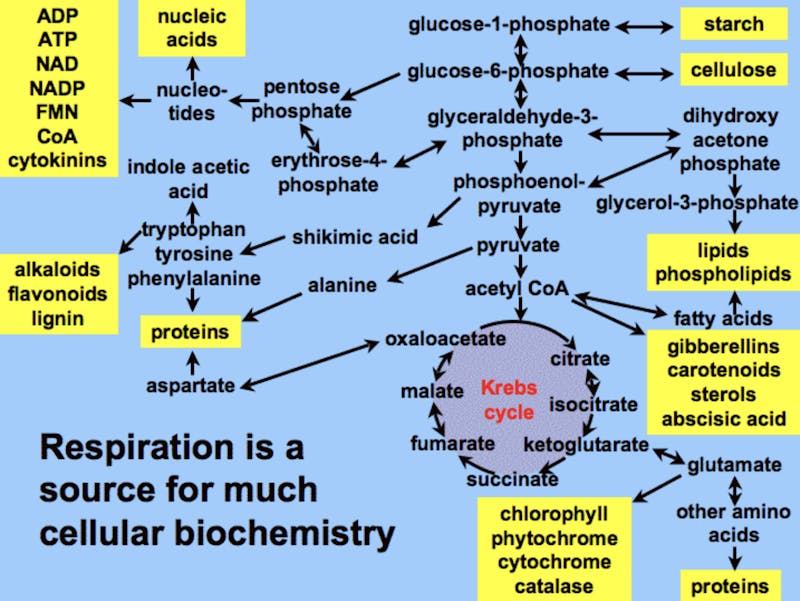
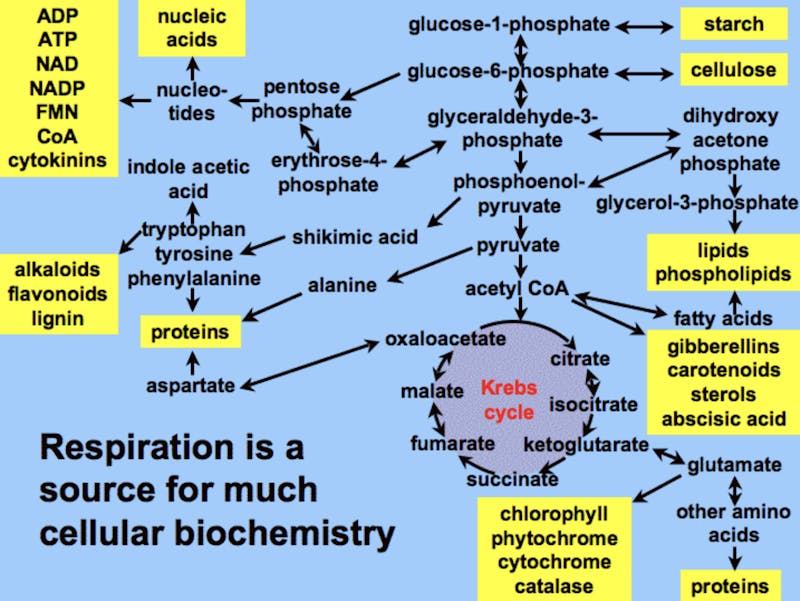
A calorie of carbohydrate is metabolized entirely differently from fat or protein. So why pretend they are the same? It’s like saying that humans and a tree trunk share the same physiology because we both weigh the same and would produce the same heat if burned in a calorimeter. Believing this notion is a big part of why we’re losing the war on obesity.
This notion of ‘A calorie is a calorie’ is mostly pushed by processed-food companies trying to convince you that it is fine to swap 100 calories of avocado for Coke in terms of weight gain. For food companies, the calories model is like Santa Claus. As long as they keep people believing, its a gift that keeps on giving. They can sell sugary beverages and tell people with a straight face that 100 calories of sugar is as fattening as 100 calories of kale.Why ‘caloric reduction as primary’ does not work
Suppose our house thermostat is set to 72F (22C) degrees, but we now want to be at 70F (21C). Ignoring the thermostat, we turn on the portable air conditioner in. At first, the temperature drops to 70F (21C) but then the thermostat turns up the heat to return the room to 72F (22C). We don’t like that, so we put a second and third air conditioner in. In response, the thermostat turns the heat on full blast. We continually fighting against ourselves in an ultimately futile attempt. Well, that didn’t work. What is a simpler solution? Turn down the thermostat.
This is analogous to reducing calories to lose weight because it completely ignores the BSW. Suppose our BSW is set at 200 pounds (91 kg), but we want to weigh 170 pounds (77 kg). Conventional advice tells us to cut 500 calories per day to lose 1 pound per week. Initially weight goes down to 185 pounds (84 kg), but then our appestat kicks in to make us gain weight. We become hungrier and basal metabolism slows in order to regain the weight. So we try even harder by cutting more calories. But our body responds by further slowing our metabolism. We continually fight against ourselves in an ultimately futile attempt to lose weight. Well, that didn’t work. What is a simpler solution? Turn down the appestat or BSW. How to do that? Read on, my friend.
The body weight ‘thermostat’
So how does our appestat work? Recall that excessive insulin continbutes to obesity in addition to excessive calories. It is a hormonal imbalance. If you are not familiar with these ideas, you can find details in The Obesity Code book or review my past blogs at www.IDMprogram.com. If you need further help, you can contact us for personalized coaching or join our membership program. Insulin signals our body to store food energy in the form of body fat. When we fast, and insulin goes down, we burn some of that stored energy and this is why we don’t die in our sleep every night.
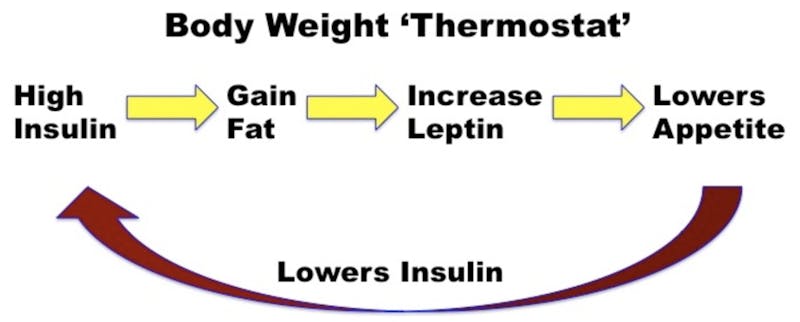
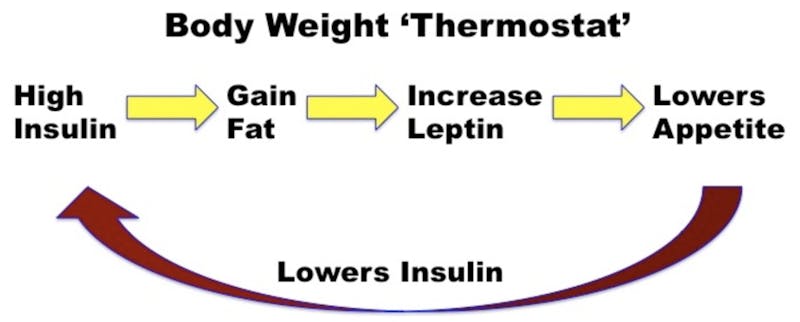
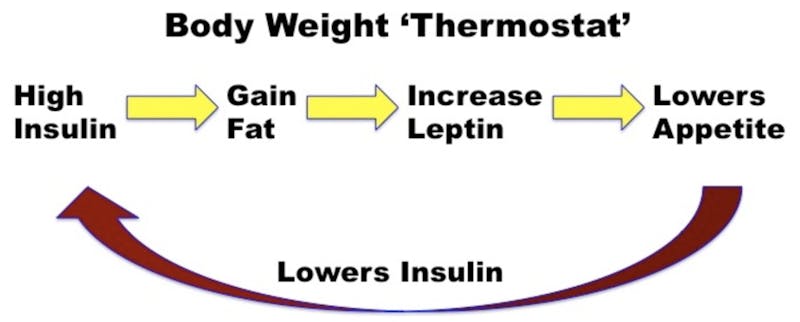
A thermostat works on a negative feedback loop. If the temperature is too low, the thermostat turns on the heat until it gets to the proper temperature and then it stops. The body also uses a negative feedback loop in the BSW. Excessive insulin leads an increase in the size of fat cells. They produce more of the hormone leptin which travels to the brain and signals that ‘we’re too fat’. Appetite decreases, we stop eating, and this lowers insulin. This signals our body to start burning fat instead of eating and storing it and returns us to our original, desired BSW.
This feedback loop keeps our weight relatively stable despite wide fluctuations in calorie intake and calorie expenditures day after day, week after week and year after year. After all, most people become obese by gaining 1-2 pounds (0.5-1 kg) per year. Over 40 years, this can add up. Assume that 1 pound (0.5 kg) of body fat is roughly 3500 calories. In a year, we might eat 2000 cal/day times 365 days = 730,000 calories. To gain 1 pound (0.5 kg) a year (3500 calories), we would need to accurately match calorie intake and expenditure to a 99.5% accuracy rate. That’s impossible. I have maintained an even weight since grade school, but I have no idea how many calories I eat and how many I expend. How do I maintain a 100% accuracy rate? Clearly, I could not do this through conscious regulation of my food intake/ exercise. No, body fat is regulated by a feedback mechanism – the BSW ‘thermostat’.
Obesity is therefore not just a caloric balance problem, but rather the gradual increase in the BSW thermostat (appestat) over time. Let see how that works.Obesity
The BSW is likely created by the balance of insulin effect versus leptin effect, just as the thermostat is regulated by the balance of heat versus cooling. In those who are obese, it is likely that the insulin effect has prevailed over leptin effect. For example, if we inject exogenous insulin, we gain fat because we have tilted the balance towards insulin. In normal human obesity, this could be due to a number of reasons, but eating foods high in refined grains, eating frequently, eating lots of sugar (causes hepatic insulin resistance directly) are all culprits in keeping insulin levels high despite leptin’s best efforts to curb appetite to lower insulin. If insulin is extremely low, as in type 1 diabetes, the body loses weight continuously no matter how many calories are eaten.
But obesity is commonly a disease caused by too much insulin – hyperinsulinemia. If you are obese, it may be because insulin prevailed over leptin. As the fat cells stay over-filled, they produce more and more leptin in an attempt to fight insulin. This should help in the Battle Royale. And it does, often for decades. However, the root problem of hyperinsulinemia has not been solved (eating too much sugar, too many refined carbohydrates, eating constantly), so insulin also continues to march higher. And persistent high levels of hormones result in resistance. Eventually, persistent, high levels of leptin cause leptin resistance. Persistent high levels of insulin cause insulin resistance. But just as true – persistent high leptin levels cause leptin resistance.
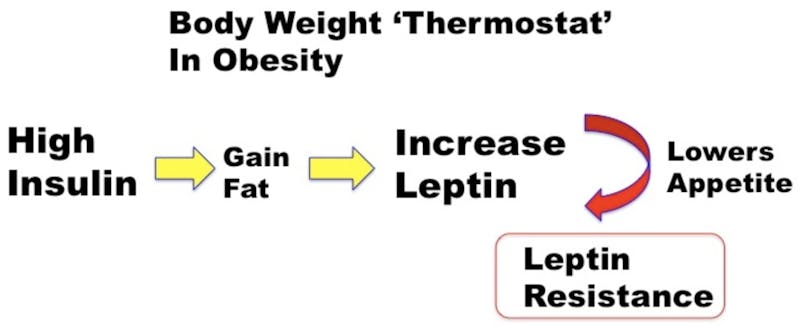
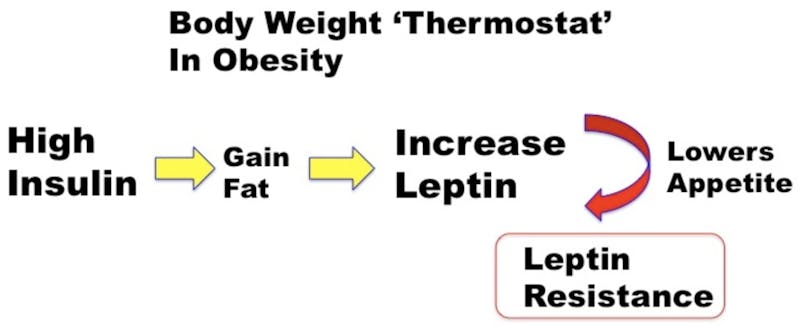
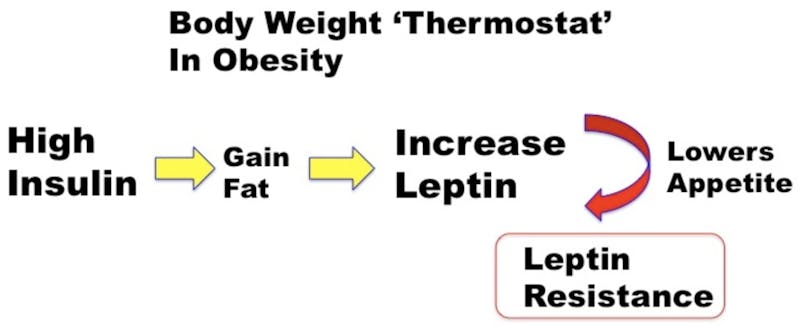
This leptin resistance is virtually universal in common obesity. With leptin down and out, insulin is now unopposed to cause weight gain. The insulin vs. leptin battle has been lost, and the BSW thermostat is reset upwards.
So, what’s the answer? Suppose we use the standard dietary advice of cutting dietary fat, reducing calories but eating lots of carbohydrates and eating 6 or 7 times per day. Since dietary fat has little insulin effect, this caloric-reduction strategy may not reduce the insulin effect and may make little difference to this Insulin vs. Leptin battle. The BSW can be unaffected and our bodies desperately try to regain the lost weight. This is precisely the dietary advice given over the last 40 years that has failed so spectacularly. Eating frequently means constant stimulation of insulin, which is also detrimental to weight loss efforts.
The key to combating obesity, then is to help in the Insulin vs. Leptin fight by lowering insulin. Everything depends upon it. Leptin is already maxed out. The only thing left is to lower insulin. How to do that? Well:
- Eat less sugar
- Eat less refined grains
- Eat adequate protein and fon’t avoid natural fats
- Don’t eat all the time (time restricted eating or intermittent fasting). Stop snacking
- Eat real unprocessed foods (lower in insulin effects)
Funny. That’s precisely the sort of no-nonsense advice your grandmother would have given. Low Carb Healthy Fats + Intermittent Fasting. Boom.
—
Dr. Jason Fung
Dr. Fung’s top posts about weight loss
Weight loss
Calories
Dr. Fung
More with Dr. Fung
Dr. Fung has his own blog at idmprogram.com. He is also active on Twitter.
Dr. Fung’s books The Obesity Code and The Complete Guide to Fasting are available on Amazon.