What and when to eat to reduce insulin

Here’s a startling truth. I can make you fat. Actually, I can make anybody fat. How? I simply prescribe insulin injections. Giving people extra insulin inevitably leads to weight gain. In type 1 diabetes, when insulin levels are extremely low, patients lose weight no matter how many calories they eat. Give insulin – gain weight. No insulin – lose weight (even to the point of death). The implication is clear. Insulin causes weight gain. Knowing this is crucial, because if insulin causes weight gain, then lowering insulin should help with losing weight. But this very different than just counting calories.
The standard (failed) weight loss advice is to restrict a few calories every day by reducing dietary fat and eating multiple times per day. This does not lower insulin much since dietary fat has little insulin effect and eating frequently constantly stimulates insulin secretion. This ‘caloric reduction as primary’ advice has an astounding failure rate. So, if you have tried calorie restriction to lose weight and failed, you are not alone.So here’s the situation. ‘Medicine’ tells you that obesity is a caloric balance problem and that you should eat less and move more. ‘Medicine’ tells you to eat a low-fat diet, and to eat six or more times a day. This advice doesn’t work for most people. When it doesn’t work, ‘Medicine’ frequently assumes it’s your fault for not being able to stick with the advice. Our advice was good, ‘Medicine’ tells you. You just didn’t do it right.
Imagine, though we have a classroom of 100 pupils. One fails. It’s likely his fault. Maybe he played too many video games. But if 99 students fail, then it’s not a problem with the students. The problem is with the teacher. In obesity, the problem of rampant obesity means that it is obviously not the fault of the people. The fault lies with the official dietary advice.
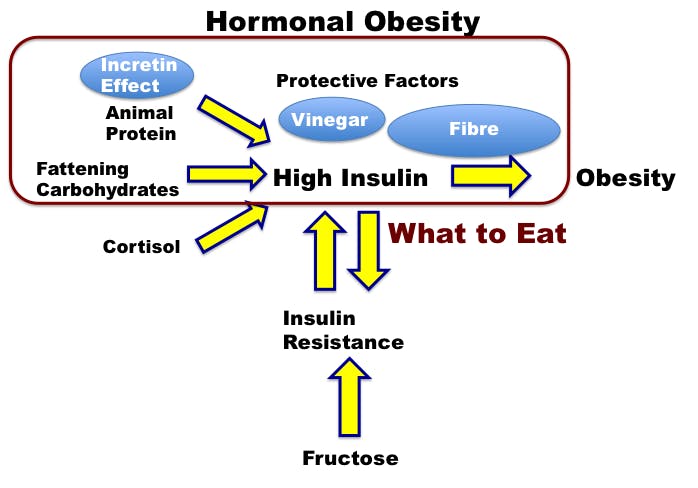
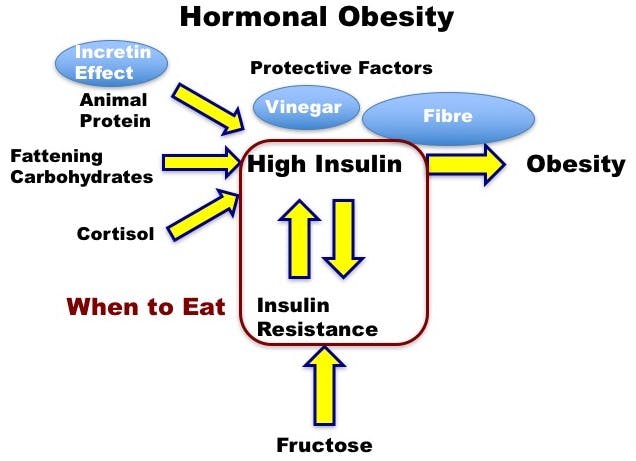
Understanding that obesity is as much a hormonal disorder as it is a caloric imbalance (as discussed in our last post) means that we must also focus on the insulin effect rather than just the number of calories to successfully lose weight. Reducing insulin depends mostly upon 2 things:
- What you eat
- When you eat
We often think and talk about the first problem, but both are equally important in lowering insulin levels.
What to eat
The three different macronutrients stimulate insulin to different degrees. Carbohydrates, particularly refined carbohydrates raise insulin the most. Protein also raises insulin somewhat, but likely doesn’t contribute to chronic hyperinsulinemia. Dietary fat raises neither glucose nor insulin.
Most natural foods contain varying combinations of the three macronutrients and therefore raise insulin to varying degrees. For example, refined carbohydrate-rich foods like cookies have the greatest effect on raising insulin and glucose. Fat-rich foods like salmon have little effect on insulin. This differing ability to stimulate insulin means that foods also differ in their fattening effect. This is only common sense.The overlap between calories and insulin effect is what causes the confusion between the hormonal (insulin) hypothesis of obesity and the caloric hypothesis of obesity. Many people say that ‘A calorie is a calorie’, which is, of course, true. But that’s not the question I asked. The question is ‘Do all calories equally lead to weight gain’? To which the answer is an emphatic no. Insulin-stimulating foods like glucose are more likely to lead to weight gain than non-insulin stimulating foods like kale, even if you have the same number of calories.
Certain factors increase insulin which encourages weight gain. The most important factors raising insulin are refined carbohydrates and insulin resistance. Fructose, from added sugar and fruits can directly cause fatty liver and insulin resistance. This leads the body to increase insulin secretion to compensate.
Other factors decrease insulin, protecting against weight gain. Acids found in fermented foods (sauerkraut, kimchee) and vinegar can lower the insulin effect of foods. Animal protein causes the secretion of incretin hormones that slows the absorption of foods thus lowering insulin. Thus meat has both pro- and anti- insulin effects. Fibre also has the same effect of slowing absorption and insulin effect.
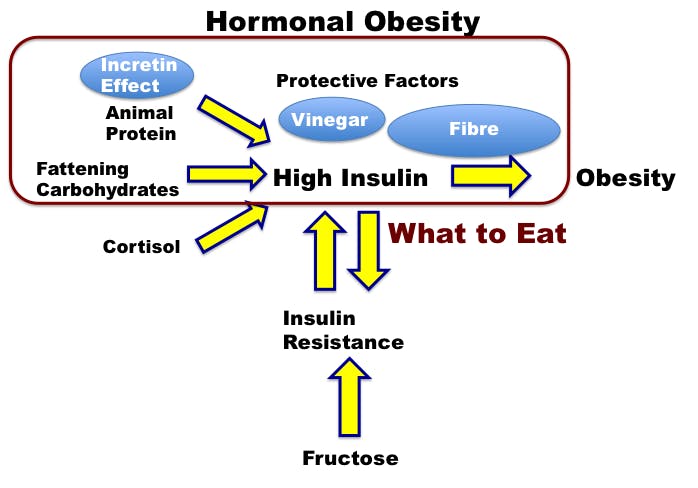
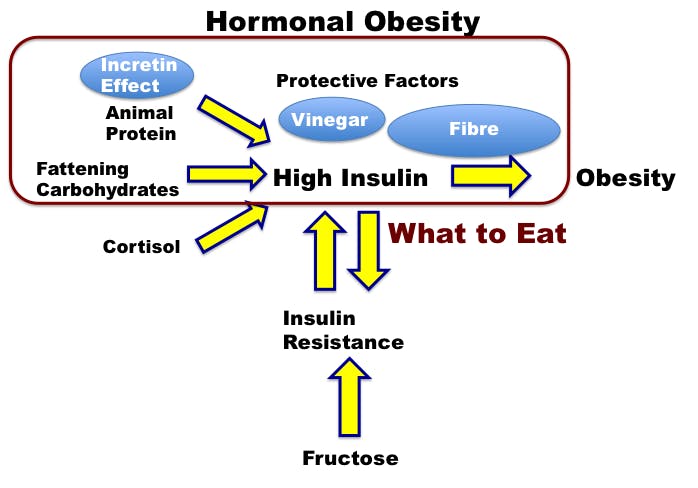
Thus, the main principles for lowering insulin and losing weight would include the following, as detailed in The Obesity Code.
Rules for ‘What to Eat’
- Avoid added sugar – causes insulin resistance and high insulin
- Eat less refined grains – High insulin effect
- Eat adequate protein
- Don’t be afraid of eating natural fats – Low insulin effect
- Eat real unprocessed foods – refining increases insulin effects
Funny. That’s precisely the sort of no-nonsense advice your grandmother would have given.
When to eat
The second and equally important part of lowering insulin is understanding the question of ‘when to eat’. All foods, aside from pure fat, can raise insulin, which can lead to obesity. But there is another important contributor to high insulin levels outside of food – insulin resistance. This refers to the situation where normal insulin levels are unable to force the blood glucose into the cells. In response, the body raises insulin in a knee-jerk reaction to ‘overcome’ this resistance, and these high levels can further drive obesity. But how did insulin resistance develop in the first place?
Our body follows the biologic principle of homeostasis. If exposed to any prolonged stimulus, the body quickly develops resistance. A baby can sleep soundly in a crowded restaurant because the noise is constant, and the baby has become noise ‘resistant’. But that same baby, in a quiet house, will wake instantly at the slightest creak of the floorboards. Since it has been quiet, the baby has no ‘resistance’ against noises and thus awakens quickly.
If you listen to loud music constantly, you will become slightly deaf. This ‘resistance’ to loud noises protects the ear from damage. Raising the volume to ‘overcome’ this resistance works but only temporarily. Volume increases and you become progressively more deaf (resistant to loud noise), which leads you to raise the volume again. The solution is not to keep raising the volume, but to shut it off.
Think about the story of the boy who cries wolf. Raising the alarm constantly may work at first but eventually leads to the villagers becoming resistant to the signal. The more the boy cries, the less effect it has. The solution is to stop crying wolf.
Insulin resistance is simply a reaction to too much insulin. The body compensates by raising insulin, but that only makes things worse because higher insulin levels lead to more resistance. This is a vicious cycle.
- High insulin leads to insulin resistance.
- Insulin resistance leads to higher insulin.
The end result is higher and higher insulin levels, which drives weight gain and obesity. Therefore, a high insulin level depends on 2 things.
- High insulin levels
- Persistence of those high levels
Providing extended periods of low insulin levels can prevent the development of insulin resistance. How to provide those low levels? Periods of fasting.
This may sound strange, but this is the way we used to eat. Suppose you eat breakfast at 8 am and dinner at 6 pm. You eat for 10 hours of the day and fast for 14 hours. This happens every single day, and the reason we use the word ‘break-fast’. This is the meal that breaks our fast implying that fasting is simply a part of everyday life. The body spends roughly equal portions of every day in the fed (insulin high, storing fat) and the fasted state (insulin low, burning fat). Because of this nice balance, weight tends to stay stable over time. Up until the 1980s, this was pretty standard practice and obesity was not a big issue.
Somehow, we moved away from this traditional way of eating and now eat constantly. We frequently eat the minute we get out of bed in the morning whether we are hungry or not, believing that eating white bread and jam or whole grain cereal is better than eating nothing at all. We eat throughout the day and don’t stop until it is time for bed. Large surveys show that most Americans eat 6-10 times per day. Now our body spends the majority of time in the fed state, and we wonder why we can’t lose weight.Eating constantly does not provide the critical period of very low insulin to balance the high insulin periods. Persistently high insulin leads to insulin resistance, which leads only to higher insulin. This is the vicious cycle of weight gain that we must break with fasting.
For the boy who cried wolf, which is the better strategy? Stop crying wolf for a month, and then cry loudly once, or cry wolf constantly, but a little more softly? Similarly, to start burning body fat, you must allow prolonged periods of time of low insulin.
Rules for ‘When to Eat’
- Don’t eat all the time (time-restricted eating or intermittent fasting). Stop snacking.
- If you want to lose more weight – increase the fasting periods
We often obsess about the foods we should or should not eat, the question of ‘what to eat’. But we often ignore the equally important question of ‘when to eat’. By attacking the insulin problem on both fronts, we have a far higher chance of successfully losing weight.
Dr. Fung’s top posts
Weight loss
Insulin
More with Dr. Fung
Dr. Fung has his own blog at idmprogram.com. He is also active on Twitter.
Dr. Fung’s books The Obesity Code, The Complete Guide to Fasting and The Diabetes Code are available on Amazon.