The seed-planting specialities

Low carb advocacy with limited time
Advocacy is when you think that you must do your part to help spread the word wider than your personal circle, that you must help correct the misinformation, and that you must start ignoring the old guard. Adapted to doctors, it could include feeling like you must convince your patients to give it a try.
But what if you are not a family physician seeing patients mainly in a clinic, and are without the option to follow them up longitudinally? What if you literally have only minutes to see each patient for their regular issues, like in subspecialised ophthalmology, or only see them in difficult contexts such as in the emergency department or on the palliative care unit?
What can you do if you believe the science supporting the low carb and keto diets, and your personal experience has convinced you of the concrete benefits for your health, weight, and well-being, and you have in front of you a patient who really should be eating low carb but obviously knows nothing about it?
I recently surveyed my medical colleagues in all specialties across Canada. If giving a full lesson on nutrition and metabolism is nearly impossible for most, the vast majority can still mention it to patients. And many do. Mentioning it is a way to advocate and spread the word.
We can call this planting seeds.
Planting seeds
 Planting seeds does not require a lot of time, but it does require a little bit of faith. You have to believe in your heart that it’s the right thing to do, whether or not you think the patient in front of you will jump on that wagon, or, should I say, whether or not you think this seed will turn into a plant and flourish.
Planting seeds does not require a lot of time, but it does require a little bit of faith. You have to believe in your heart that it’s the right thing to do, whether or not you think the patient in front of you will jump on that wagon, or, should I say, whether or not you think this seed will turn into a plant and flourish.
My own personal clinical experience has shown me I am not very good at guessing which seed will turn into a plant and which will dry up and die, or stay dormant for now. It’s very similar to counseling patients to quit smoking. The fact that our success rate isn’t 100% does not mean we should stop counselling patients to leave that poison behind.
So, across Canada, which specialities, aside from family medicine, actually counsel patients and colleagues on low carb, and how much time does it take them?
- Anesthesia, from 1 to 3 min. Before they fall asleep, that is.
- Anesthesia, working in pain clinic, around 2-3 minutes.
- Cardiac surgery, about 5-10 minutes, but not during surgery.
- Cardiology, a few minutes, to get to the heart of the problem.
- Dermatology, 5 minutes, especially with patients with acanthosis nigricans and PCOS.
- Emergency Medicine, less than 3 minutes, especially with patients with sky-high sugar levels.
- Gastroenterology, around 5-10 min, especially with patients with fatty liver and IBS.
- General Surgery, 5-10 minutes, especially for diabetes control and weight loss prior to most major surgery, in particular hernia repair.
- Gynecology, 10-15 minutes, in particular to PCOS patients, infertility patients and peri-/post-menopausal women.
- Hemato-Oncology, a few minutes, to discuss reduced risk of some malignant disease as well as the non-oncology health benefits, for example.
- Hepatology, anywhere from 5 to 40 minutes per patient! Because fatty liver, you know!
- Infectiology, a few minutes, mainly to patients with diabetes and osteitis.
- Internal Medicine, to most patients who are overweight or have diabetes, about 5 to 15 minutes, or 1h if they come specifically for dietary counselling.
- Microbiology, 5-10 minutes, mainly for obese or patients with diabetes with infected wounds.
- Ophthalmology, 5-10 minutes.
- Opiate addiction medical clinic, 5-10 minutes.
- Orthopedic, less than 3 minutes.
- Palliative care, less than 20 minutes.
- Pathology, counselling staff, family and friends, but not so much patients, for obvious reasons….
- Pediatrician, a few minutes.
- Peds neuro, a few minutes, especially to migraine patients.
- Physiatry, less than 5 minutes, often to migraine patients.
- Plastic surgery, 5-10 minutes, to numerous patients.
- Psychiatry, about 10-20 minutes.
- Radiology, usually while performing an ultrasound (fatty liver) or biopsy, around 5-15min, if not less than 1 minute. Captive audience!.
- Respirology/sleep medicine: about 1-5 minutes.
- Rhumatology, around 5 minutes per patient.
- Other specialties not listed here: they may not have seen my post!



The one-minute speech
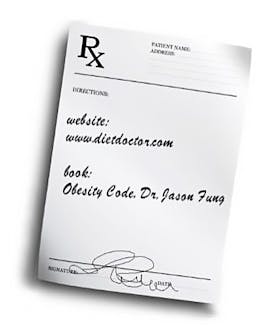
If all you have is that one encounter with the patient in front of you, give them at least a one-minute speech, and resources. Plant that seed.
Here’s a one-minute speech from Dr. David Unwin, general practitioner in the UK, quoted with his permission:
You have multiple chronic health problems. All of which are associated or caused by lifestyle habits. There are a couple of ways we can go at this point: continue down the lifelong medication route, and you’ll probably need more meds overtime, and we’ll see how that goes, or there is a very promising alternative pathway, which is looking at diet. I’ll give you a diet sheet, and if you stick to it, we probably won’t need more meds. In fact, we may even be able to deprescribe some of them. You will probably lose weight, you will probably feel less hungry, and you’ll probably feel better.
Which do you want to choose?
Doctors from all specialties can make a difference
Any doctor from any specialty can adapt this simple speech to suit their context, and have a prescription pad with a few resources already printed on it. It really doesn’t need to take a lot of time. But it makes a difference, whether you end up seeing the results or not.



So, plant that seed whenever you can. And have a little faith.
More
Earlier with Dr. Bourdua-Roy
All earlier posts by Dr. Bourdua-Roy