Is a keto diet helpful for migraines and cluster headaches?
If you suffer from migraines or cluster headaches, you’ll likely agree that few things on earth can make you feel more miserable. Could following a ketogenic diet possibly provide relief?
Emerging scientific evidence suggests that, possibly by reducing inflammation in the brain, keto eating may benefit those with migraines or cluster headaches.1 Indeed, some people have reported that their headaches dramatically improved after switching to a keto diet.
In this guide, we’ll discuss why a ketogenic diet may be helpful for migraines and cluster headaches, and provide practical advice for getting the best results.
What are migraines?
In most cases, migraine headaches, or migraines, cause severe pain — often described as throbbing or pulsating pain — in the front, side, or back of the head; they typically last between four and 72 hours. However, a minority of migraines have “atypical symptoms” not associated with pain.
In addition to pain, a migraine attack usually includes other debilitating symptoms, such as:
- Nausea and vomiting
- Dizziness
- Blurred vision
- Extreme sensitivity to light, sounds, and odors
It’s estimated that approximately 1 billion people — or nearly 1 in 8 — worldwide experience migraines.3 These headaches affect about twice as many women as men, and fluctuating estrogen levels at puberty and during the menstrual cycle are known migraine triggers.4 Many other things can potentially trigger migraines in susceptible people, such as:5
- Certain foods (chocolate, cheese, alcohol, artificial sweeteners, and food additives are common offenders, although responses vary among individuals)
- Dehydration
- Lack of high-quality sleep
- Stress
- Changes in weather and barometric pressure
Triptans and other medications can provide relief during acute attacks, while anticonvulsant drugs and other medication classes may help prevent migraines. However, these therapies often cause unpleasant side effects.8 Additionally, some people may develop drug-resistant migraines.9
Summary
Migraines are severe headaches that are usually accompanied by nausea, dizziness, and sensitivity to light and noise. They are more common in women and can be triggered by hormonal changes, certain foods, stress, and other factors. Medications provide relief for some but often come with side effects.
Keto for migraines
Why a ketogenic diet might help
Despite years of research, the exact mechanisms behind migraine headaches are still not completely understood. However, they’re believed to involve inflammation, chemical imbalances, and impaired energy metabolism in the brain.10
Some researchers suggest that, as a response to an energy deficit or chemical imbalance in the brain, the migraine attack itself may be the brain’s attempt to restore proper balance.11
Epilepsy is another neurological disorder that appears to be related to migraines and may potentially have similar mechanisms.12
For decades, ketogenic diets have been used to treat epilepsy and are now considered an approved therapy in individuals who don’t respond to anticonvulsant drugs.13
Some experts are now suggesting that a ketogenic diet may work similarly for migraines. In addition to providing an alternative energy source for the brain, ketones may reduce inflammation and beneficially influence other factors believed to play a role in migraines.14
Summary
Migraines appear to involve inflammation, chemical imbalances, and impaired energy metabolism in the brain. Some researchers theorize that ketogenic diets may provide migraine relief by reducing inflammation and imparting other beneficial effects to the brain.
Scientific evidence supporting keto diets for migraines
Research on the ketogenic diet for migraines is sparse — and nearly all of it has been overseen or conducted by the same team of Italian researchers.
In 2013, they published a case study of adult twin sisters with frequent migraines who were following a cyclical ketogenic diet to lose weight. For nine months, they alternated between eating a keto diet for one month and a low-calorie, lower-carb diet for two months.
Eating this way not only allowed the sisters to reach their weight loss goals but also led to an unexpected — but very welcome — dramatic reduction in the frequency and severity of their migraines during the keto periods of the diet.15
Next, the researchers arranged an observational study in 96 overweight women with migraines at a local clinic. Participants received advice from a dietitian to follow either a standard low-calorie diet for six months or a low-calorie ketogenic diet for one month and a standard low-calorie diet for five months.
The first month, women in the keto diet group had significantly fewer headaches and used far less migraine medication than the standard low-calorie diet group. Once the keto group began eating the standard low-calorie diet, their migraine attacks increased, although they remained lower than at baseline.16
In 2019, the research team conducted a randomized crossover trial in 35 overweight adults with migraines who followed a low-calorie ketogenic diet and a low-calorie non-ketogenic diet for one month each. Migraine frequency decreased by 50% or more in 26 people during the keto diet, but only in three people during the non-keto diet.17
In a non-controlled trial published the same year, the researchers studied brain activity changes in 18 people whose migraines became less frequent after eating a ketogenic diet for one month. They concluded that the diet appeared to help normalize brain activity in the participants.18
Another non-controlled trial from a different team in Italy demonstrated a significant reduction in headache frequency and duration in subjects trying a ketogenic diet.19
And finally, a retrospective study reported that keto’s beneficial effects on migraine symptoms appeared unrelated to weight loss, and therefore likely represent a direct beneficial effect from ketosis.20
Although promising, these are small studies from a limited group of researchers. More trials are needed to determine the ketogenic diet’s effects in people with migraines.
Summary
In small studies, ketogenic diets have been found to reduce the frequency and severity of migraines, leading to decreased use of medication in some of the participants. However, improvement didn’t occur in everyone. More studies – especially clinical trials – are needed.
Anecdotal evidence supporting keto diets for migraines
In recent years, stories of people experiencing fewer and less severe migraines after adopting a keto diet have been increasing.
In some, like the twin sisters in the case study, migraine improvement was an unanticipated side benefit of the keto diet.
Here are a few stories from people who have experienced fewer migraines — in addition to losing weight and seeing other positive health changes— by following a keto lifestyle:
We also have an inspirational video interview with migraine researcher Elena Goss, whose own debilitating migraines led her to adopt the ketogenic diet:
Getting started
How can you follow the keto diet and get the best results for migraines? Here are a few pointers:
- Keep carbs very low: At Diet Doctor, we define a keto diet as one that contains 20 or fewer grams of net carbs per day.21 It’s possible that you might be able to eat slightly more carbs and still achieve relief from migraines.22 But since keeping your daily net carb count under 20 virtually guarantees you’ll be in ketosis, it’s a good place to start.
- Learn more about the keto diet: Check out our comprehensive keto diet guide for more detailed information and answers to common questions about keto.
- Take steps to avoid the “keto flu:” When first starting a ketogenic diet, some symptoms are fairly common, including headache. Our keto flu guide can help you minimize or possibly even prevent these side effects. Boosting your salt and water intake can be especially helpful.
- Get enough magnesium: A review of 21 randomized trials found that taking oral magnesium may alleviate the frequency and severity of migraine.23 Consider supplementing with up to 400 mg per day, or simply eat keto foods that are high in magnesium, such as leafy greens, fatty fish, nuts, and seeds.
- Discuss medications with your doctor: If you are currently taking medications for migraines, consult your doctor before making any medication changes.
- Diet Doctor can give you support along the way. We have a free two-week Get Started Keto Challenge that provides everything you need, including encouraging emails, meal plans, and shopping lists.
Sign up for our FREE Get Started Keto Challenge!
What are cluster headaches?
Like migraines, cluster headaches can cause severe pain. However, they only occur on one side of the head, around the eye or temple. Additionally, the excruciating pain is described as “stabbing” rather than “throbbing.”
These headaches are so named because they come in “clusters” up to eight times per day, with each episode lasting between 15 minutes and three hours.
Cluster cycles typically last anywhere from a few days to a few months, with several months of remission between episodes. These are considered “episodic” cluster headaches.
However, in about 10-15% of cases, the headaches become chronic, persisting for a year or more with either no remission period or remission periods lasting less than one month.24
Additional symptoms can include a runny nostril, teary eye, and flushed skin on the affected side of the face.
Although they’re considered relatively rare, cluster headaches occur in an estimated 1 in 1,000 people worldwide.25
They’re diagnosed based on the clinical features of the attack — severe cyclical pain confined to one side of the head — along with ruling out other causes.
Like migraine headaches, cluster headaches can be triggered by alcohol (especially red wine), chemicals, stress, or weather changes.26 And like migraines, cluster headaches can be disabling and greatly impact quality of life.27
Treatments during acute attacks include inhaling oxygen and taking triptan drugs. Calcium channel blockers and steroids are sometimes used to help prevent attacks during a cluster period. Yet, like migraine treatment, some people experience side effects or don’t respond to these medications.28
Summary
Cluster headaches cause severe one-sided head pain several times a day for a few days, weeks, or months. In chronic cluster headaches, attacks can last for a year or longer. Triggers include alcohol, chemicals, stress, and weather changes. Acute and preventive treatments may help some but not all people with cluster headaches.
Keto for cluster headaches
Why a ketogenic diet might help
The mechanism behind cluster headaches remains unknown. However, like migraines, inflammation seems to play a role.29
Although they are separate conditions with unique symptoms, migraines and cluster headaches have similar triggers. Moreover, they’ve been found to share other features, including brain chemical imbalances and changes in brain steroid levels.30
Given the early evidence supporting ketogenic diets in some people with migraines, it’s possible that this way of eating may also be helpful for individuals with cluster headaches.31
Summary
Ketogenic diets can potentially reduce inflammation, and small studies suggest they may be beneficial for people with migraines. Because migraine and cluster headaches share some similarities, a keto approach may potentially provide relief for people with cluster headaches.
Scientific evidence supporting keto for cluster headaches
Published research on ketogenic diets for cluster headaches is extremely limited. To date, there are only two studies, and both were conducted by the same team of Italian researchers who have published studies on the ketogenic diet for migraines.
In the first trial, 12 people with drug-resistant cluster headaches ate a ketogenic diet for 12 weeks. By the end of the study, all five participants with episodic cluster headaches became symptom-free, and six out of seven with chronic cluster headaches experienced an improvement in symptoms.32
Interestingly, the researchers reported that all participants with episodic cluster headache remained symptom-free even after they resumed eating a standard diet, although they did not specify for how long the participants were followed after the trial.
In a similar small trial, 18 people with drug-resistant chronic cluster headaches consumed a ketogenic diet for 12 weeks. By the end of the study, 11 participants became symptom-free, and four others had a 50% or greater reduction in monthly headaches.33
Results from these small trials are encouraging, but more studies from other researchers are needed to establish the efficacy of ketogenic diets for cluster headaches.
Summary
Limited research suggests that keto diets may help reduce or possibly resolve cluster headaches in people with drug-resistant cluster headaches. However, much more study is needed.
Anecdotal evidence supporting keto for cluster headaches
Because cluster headaches are far less common than migraines, it’s a bit tougher to find reports of cluster headache improvement in those who have tried keto eating.
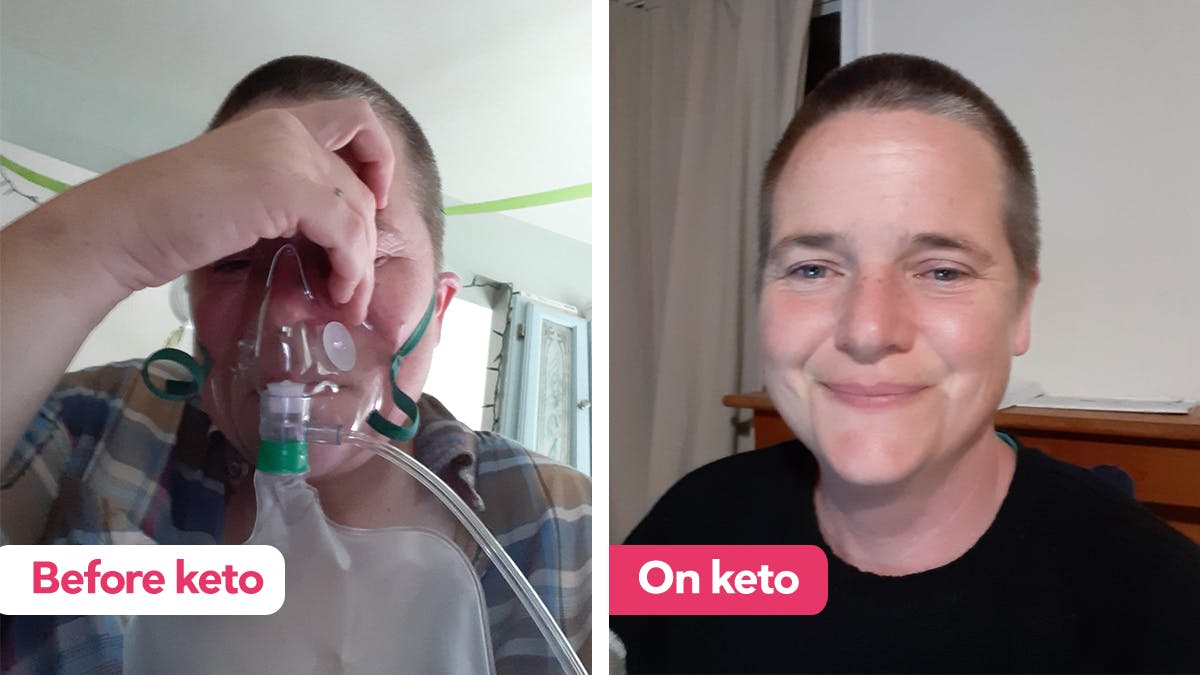
Recently, we featured the story of a woman who suffered from cluster headaches for more than 16 years until she began eating a keto diet three months ago. While she previously had at least three headaches a day, Karen says she hasn’t had a single headache in over two months.
Getting started
If you’re interested in following a keto diet for cluster headaches, check out our keto diet guide for beginners. Also, be sure to follow our tips to help you minimize symptoms of the keto flu (one of which is headaches).
If you’d like some support along the way, we also have a free two-week Get Started Keto Challenge that provides everything you need, including encouraging emails, meal plans, and shopping lists.
Finally, be sure to discuss medications with your doctor before starting a keto diet.
Key takeaways
If you suffer from migraines or cluster headaches, a keto diet may potentially help improve your symptoms.
Based on published studies and personal reports, some people have experienced dramatic reductions in headache frequency, severity, and medication usage simply by changing their diet.
However, there are no guarantees. As with epilepsy and other neurological conditions, it’s likely that not everyone who follows a keto diet for migraine or cluster headaches will improve.
On the other hand, a keto diet is a healthy way of eating that can provide other benefits. And if following a keto lifestyle might lead to fewer migraine or cluster headaches and improve your quality of life, it seems worthwhile to give it a try.
/ Franziska Spritzler, RD, CDE
Learn how to do a keto diet
Is a keto diet helpful for migraines and cluster headaches? - the evidence
This guide is written by Franziska Spritzler, RD and was last updated on June 19, 2025. It was medically reviewed by Dr. Michael Tamber, MD on October 19, 2021 and Dr. Bret Scher, MD on October 3, 2022.
The guide contains scientific references. You can find these in the notes throughout the text, and click the links to read the peer-reviewed scientific papers. When appropriate we include a grading of the strength of the evidence, with a link to our policy on this. Our evidence-based guides are updated at least once per year to reflect and reference the latest science on the topic.
All our evidence-based health guides are written or reviewed by medical doctors who are experts on the topic. To stay unbiased we show no ads, sell no physical products, and take no money from the industry. We're fully funded by the people, via an optional membership. Most information at Diet Doctor is free forever.
Read more about our policies and work with evidence-based guides, nutritional controversies, our editorial team, and our medical review board.
Should you find any inaccuracy in this guide, please email andreas@dietdoctor.com.
Nutrients 2019: Potential protective mechanisms of ketone bodies in migraine prevention [overview article; ungraded]
The Journal of Headache and Pain 2015: Cluster headache improvement during ketogenic diet [non-controlled study; weak evidence] ↩
Journal of Headache and Pain 2019: Neuroimaging clues of migraine aura [review article; ungraded] ↩
The Lancet Neurology 2018: Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016 [systematic analysis; ungraded] ↩
Current Opinion in Neurology 2014: Migraine and estrogen
[review article; ungraded] ↩Current Pain and Headache Reports 2014: Migraine and triggers: Post hoc ergo propter hoc? [review article; ungraded] ↩
Headache 2017: Chronic migraine: An update on physiology, imaging, and the mechanism of action of two available pharmacologic therapies [review article; ungraded] ↩
Neurology Clinics 2019: Migraine: epidemiology, burden, and comorbidity [review article; ungraded] ↩
One paradoxical side effect is a headache that occurs from medication overuse:
Expert Opinion on Drug Metabolism & Toxicology 2018: Side effects associated with current and prospective antimigraine pharmacotherapies [review article; ungraded] ↩
Neurotherapeutics 2018: Non-pharmacological approaches for migraine [review article; ungraded] ↩
The Journal of Headache and Pain 2019: Mechanisms of migraine as a chronic evolutive condition [Review article; ungraded]
Brain 2017: Cortical glutamate in migraine [observational study; very weak evidence]
Current Medicinal Chemistry 2019: Energy metabolism impairment in migraine [Review article; ungraded] ↩
Nature Reviews. Neurology 2019: The metabolic face of migraine – from pathophysiology to treatment [overview article; ungraded] ↩
These include higher concentrations of excitatory neurotransmitters and impaired functioning of the sodium and potassium ion channels responsible for conducting nerve impulses:
Neurological Sciences 2017: Shared mechanisms of epilepsy, migraine and affective disorders [Review article; ungraded] ↩
Randomized controlled trials (RCTs) have shown that ketogenic diets can be very effective for seizure control in some, although not all, children and adults with epilepsy:
Epilepsia 2018: Effect of modified Atkins diet in adults with drug-resistant focal epilepsy: a randomized controlled trial [moderate evidence]
Acta Neurologica Scandinavica 2017: A randomized controlled trial of the ketogenic diet in refracatory childhood epilepsy [moderate evidence]
Epilepsy Research 2016: Evaluation of a simplified modified Atkins diet for use by parents with low levels of literacy in children with refractory epilepsy: a randomized controlled trial [moderate evidence] ↩
Beta-hydroxybutyrate, the most prevalent ketone body, is a signaling molecule that may help reduce neuron excitability and maintain biochemical balance in the brain:
Nutrients 2019: Potential protective mechanisms of ketone bodies in migraine prevention [overview article; ungraded] ↩
During the non-keto periods, the women’s migraine symptoms returned, although they were less frequent and intense than they had been before starting the diet:
Functional Neurology 2013: Diet transiently improves migraine in two twin sisters: possible role of ketogenesis? [case study; very weak evidence] ↩
By the end of the study, migraine frequency and medication usage was lower in both groups of women compared to baseline. However, all migraine parameters improved the most during the one month of ketogenic eating:
European Journal of Neurology 2015: Migraine improvement during short lasting ketogenesis: a proof-of-concept study [observational study; weak evidence] ↩
Nutrients 2019: A randomized double-blind, cross-over trial of very low-calorie diet in overweight migraine patients: a possible role for ketones? [randomized crossover trial; moderate evidence] ↩
Specifically, the study found that the keto diet reduced cortical excitability, suggesting that the cerebral cortex may be the primary site of KD-modulation.
BioMed Central Neurology 2019: A ketogenic diet normalizes interictal cortical but not subcortical responsivity in migraineurs [non-controlled study; weak evidence] ↩
Neurological Sciences 2021: Effectiveness of ketogenic diet in treatment of patients with refractory chronic migraine [non-randomized study; weak evidence] ↩
Journal of Clinical Medicine 2022: Migraine prevention through ketogenic diet: More than body mass composition changes ↩
Net carbs = total carbs minus fiber ↩
In studies investigating the ketogenic diet for migraines, participants have achieved improvement when eating 15 to 30 grams of net carbs per day:
BioMed Central Neurology 2019: A ketogenic diet normalizes interictal cortical but not subcortical responsivity in migraineurs [non-controlled study; weak evidence]
Nutrients 2019: A randomized double-blind, cross-over trial of very low-calorie diet in overweight migraine patients: a possible role for ketones? [randomized trial; moderate evidence]
European Journal of Neurology 2015: Migraine improvement during short lasting ketogenesis: a proof-of-concept study [non-controlled study; weak evidence] ↩
Pain Physician 2016: Effects of intravenous and oral magnesium on reducing migraine: a meta-analysis of randomized controlled trials
[systematic review of randomized trials; strong evidence] ↩Journal of Neurology 2019: Cluster headache: pathophysiology, diagnosis and treatment [overview article; ungraded] ↩
Cephalagia 2008: The incidence and prevalence of cluster headache: a meta-analysis of population-based studies [review article; ungraded] ↩
Journal of Neurology 2019: Cluster headache: pathophysiology, diagnosis and treatment [overview article; ungraded] ↩
In a study of 224 people with cluster headaches, 85% of the participants were considered to be severely impacted by the condition:
Scientific Reports 2020: Clinical factors influencing the impact of cluster headache from a prospective multicenter study [cross-sectional study; weak evidence] ↩
The Journal of Headache and Pain 2014: Refractory chronic cluster headache: a consensus statement on clinical definition from the European Headache Federation [consensus statement; ungraded] ↩
Journal of Neurology 2019: Cluster headache: pathophysiology, diagnosis and treatment [overview article; ungraded] ↩
The Journal of Headache and Pain 2018: Migraine and cluster headache – the common link [overview article; ungraded]
Journal of Headache and Pain 2019: Migraine and cluster headache show impaired neurosteroids patterns
[observational study; weak evidence] ↩As we detail below in the section on scientific evidence, research investigating ketones and cluster headaches is limited ↩
The Journal of Headache and Pain 2015: Cluster headache improvement during ketogenic diet [non-controlled study; weak evidence] ↩
Frontiers in Neurology 2018: Efficacy of modified Atkins ketogenic diet in chronic cluster headache: an open-label, single-arm, clinical trial [non-controlled study; weak evidence] ↩