The ketogenic diet for Alzheimer’s prevention and treatment: can it help?
If you’re like most individuals, you fear developing Alzheimer’s Disease as you age.Aging is hard enough as it is – losing strength and vitality, having your hearing and eyesight decline, often developing other health problems. But when aging includes losing your memory and cognitive function, being unable to recognize family and friends, by losing one’s way in your own neighborhood or home, losing your sense of self, it can strike fear and despair.
Most people would do anything to try to avoid dementia.
Could a low carb or keto diet help protect your brain from the ravages of aging? Could increasing ketones in your blood help spare your memory or reduce your risk of developing Alzheimer’s Disease?
This guide provides an evidence-based review of what we know about Alzheimer’s and how a ketogenic or low carb diet may help. It ends with a small family experiment I did with my elderly parents in 2018.
Alzheimer’s and other dementias — the growing scourge
Alzheimer’s Disease and other related neurodegenerative conditions — which impact memory, behavior and decision-making — are now epidemic in Western societies.
Currently an estimated 50 million cases of Alzheimer’s and dementia exist globally, including 7.5 million in Western Europe and 5 million in North America. Those numbers are expected to increase by more than 200% over the next 30 years, reaching 150 million cases worldwide by 2050.1
Modifiable risk factors for Alzheimer’s include type 2 diabetes, obesity, metabolic syndrome, and high blood pressure.2 Research has shown that these risk factors may be controlled or improved with a low-carb or ketogenic lifestyle.3
One risk factor that is impossible to change is increasing age. The older you grow, the higher your risk of dementia. And with each passing year after entering the late 80s the incidence of dementias increases exponentially, reaching upwards of 40% by age 100.4
At this time there is neither a cure nor an effective treatment. Research for the last two decades has been burgeoning and more than 3,600 clinical trials for various interventions are currently underway around the world, including studies in various phases for more than 100 new drugs.5 Yet the track record for drug effectiveness has been dismal.6
Because rates of Alzheimer’s have increased so dramatically, many people in middle to older age report being concerned that they may develop it or other forms of dementia.7
With so little in the way of effective treatment, many who fear Alzheimer’s are motivated to try diet and lifestyle changes. If a ketogenic diet has even the slimmest chance of offering a positive impact, they want to know.
The brain likes ketones
It has long been known that the brain can use ketones to meet a large portion of its fuel needs.8 Your liver creates ketones from fatty acids, either from fat in your diet or fat stored in your body.
Although carbs break down to glucose in your digestive tract, you don’t have to eat carbs to supply your brain with the small amount of glucose it requires. This is because your liver can make all the glucose your brain needs through a process known as gluconeogenesis (literally “making new glucose”).9 Evidence that certain neurologic problems can improve by increasing the use of ketones for brain fuel has existed for almost a century.
For instance, several high-quality trials have shown that in some but not all cases, the ketogenic diet can reduce the frequency and severity of seizures in children with epilepsy.10 And a number of researchers have hypothesized that tapping into ketone metabolism may have powerful applications for many other areas of brain health.11
Diet Doctor has a number of videos and posts about positive impacts of the ketogenic diet for migraines, brain cancer, and traumatic brain injury. Anecdotally many people who adopt the ketogenic diet report improvements in their mental health, including anxiety, depression and bipolar illness.12Yet the research base, while promising, is slim by some accounts.13
While the exact mechanisms for ketones improving brain health are still unclear, a 2018 review suggests that ketones may enhance energy production, increase nerve cell growth factors, strengthen the signal sent between nerve synapses, and reduce brain inflammation.14 And a 2020 study suggested ketones “stabilize” the brain’s nerve connections while glucose destabilizes them.15
A popular book promoting the ketogenic diet for Alzheimer’s prevention is Amy Berger’s The Alzheimer’s Antidote.16 Another 2015 book, written by Dr. Mary Newport, details how she slowed her husband’s Alzheimer’s by feeding him plenty of coconut oil, MCT oil (medium chain triglycerides – derived from coconut oil, palm kernel oil and dairy products) and ketone supplements.17
Scientific evidence: Alzheimer’s brains show reduced uptake of glucose
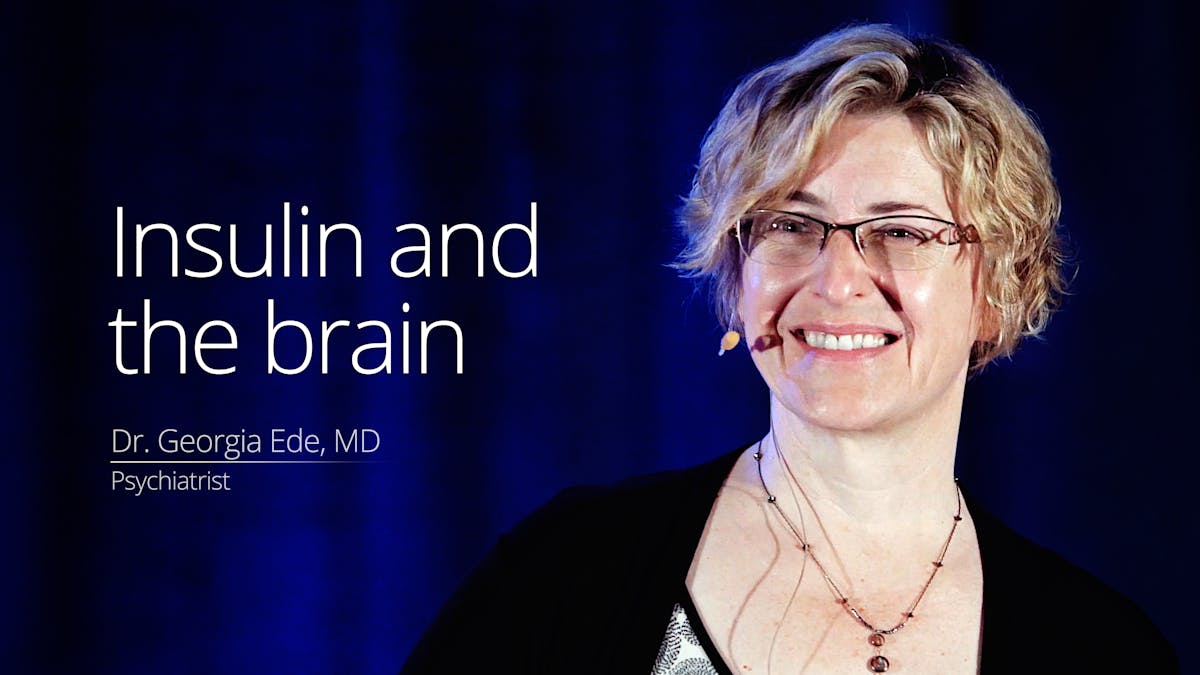
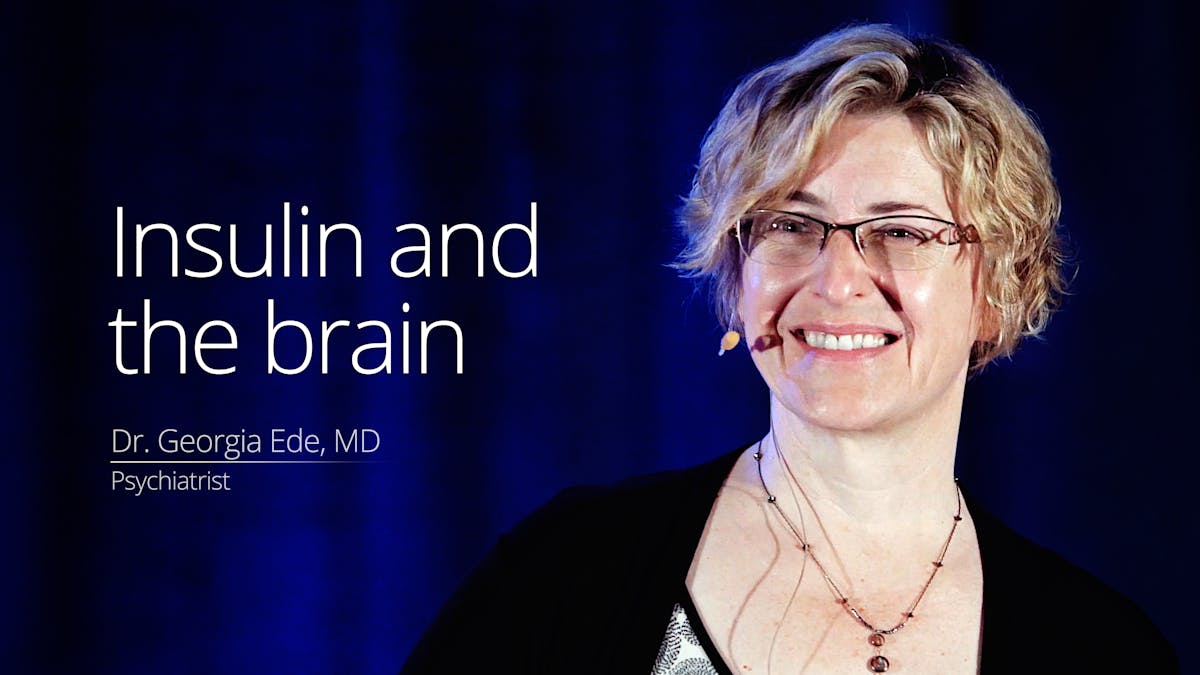
In Alzheimer’s Disease, insulin resistance (IR) in the brain may hamper the uptake of glucose for fuel, Dr. Georgia Ede notes in her 2017 video. She also delves into the issue in a related column for Psychology Today, “Preventing Alzheimer’s may be easier than you think.”
Insulin resistance of the brain as a factor associated with Alzheimer’s is so well documented that some researchers have called Alzheimer’s “type 3 diabetes.”18
This brain IR, which limits the brain’s use of glucose no matter how high blood sugar rises, may help explain the higher rates of Alzheimer’s among those with type 2 diabetes.19 For example, in a 2004 study, autopsy data revealed that 81% of people with Alzheimer’s had either type 2 diabetes or prediabetes.20 In another autopsy study, people who died with Alzheimer’s Disease had evidence of brain glucose dysregulation.21
However, brain IR may even impact the uptake of glucose in people with diabetes or prediabetes who are years away from any cognitive symptoms.22 In addition, it may affect brain glucose metabolism in young women with polycystic ovarian syndrome (PCOS).23
“We know that in Alzheimer’s Disease, the brain loses its ability to use glucose,” said Dr. Stephen Cunnane, PhD, of the University of Sherbrooke, in Quebec. Cunnane and his team are some of the world leaders using Positron Emission Tomography (PET scan) imaging, which uses glucose molecules with radioactive tags to visualize how brain cells take up sugar.
Says Cunnane, it has been known since the early 1980s, through the use of PET scanning, that brain glucose metabolism is impaired in individuals with Alzheimer’s.24
“In Alzheimer’s Disease, some areas of the brain are down by 40% in terms of glucose metabolism. We believe this energy gap increases the risk of neuronal dysfunction and cognitive decline,” Cunnane says.
Cunnane has been an author on more than 60 papers, including several examining brain energy metabolism using PET imaging, especially in Alzheimer’s Disease and other dementias. His team’s studies have found that while glucose uptake is impaired in early Alzheimer’s, the brain’s use of ketones is not.25
In a February 2018 presentation, Cunnane likens our brains to a hybrid car that can run on glucose or ketones. If it is no longer running well on glucose, it is very reasonable for people to switch the fuel to ketones, either by a ketogenic diet or by adding ketone supplements. “Attempting to treat the cognitive deficit early in Alzheimer’s using ketogenic interventions in clinical trials is safe, ethical and scientifically well-founded,” Cunnane noted in a 2016 paper.26
Early clinical trials: promising preliminary results
While the scientific rationale for using ketones in Alzheimer’s is solid, it is still seen as a very novel, unorthodox approach by many Alzheimer’s researchers and clinicians. While a number of rodent studies have been done, only a handful of ketogenic human interventions have occurred amidst thousands of other clinical trials for Alzheimer’s. In addition, there are only a few new trials in the active or recruiting stage.
Here is a summary of notable studies that have been completed so far:
- A 2021 randomized crossover study found subjects following a modified ketogenic diet (29% protein, 59% fat, and 6% net carbs) had significant improvements in quality of life and ability to perform daily activities compared to when they followed a low-fat diet.27 They also noticed excellent compliance and no increase in side effects with the ketogenic diet.
- In a 2012 study, 23 older adults with mild cognitive impairment (MCI) were randomly assigned to eat either a very low-carb ketogenic diet or a high-carb low-fat diet for six weeks. Those on the ketogenic diet lost weight and inches around their waist and also saw improvements in fasting blood sugar and insulin levels. Most importantly, performance on memory tests measurably improved in the low-carb group, with the greatest improvements among those who achieved the highest levels of blood ketones.28
- In 2018, Cunnane published his group’s results of a six-month randomized controlled trial of ketone supplementation (30 grams of MCT a day) in 17 patients with mild to moderate Alzheimer’s Disease.29 Dr. Cunnane remarked in an interview that he was encouraged to see the brain’s use of ketones increased with the 30g dose of MCT, and he suspects it may be even greater at higher doses.
- In 2016, Japanese researchers conducted a trial in 19 healthy, cognitively normal adults over the age of 60. They fed the participants a ketogenic meal with MCT oil, measured their blood ketones, and ran cognitive tests 90 and 180 minutes after the meal. Those with the worst cognitive scores prior to the keto meal showed the most improvement in working memory, visual attention and task-switching after the intervention.30
- A similar 2019 study showed no cognitive differences between participants given a single 50 gram dose of a ketogenic formula (containing 20 grams of MCT) versus control subjects fed a calorically matched placebo. However, the trial continued as a single-arm study and gave subjects 50 grams of the keto formula daily for 3 months, and some cognitive improvements were seen.31
- In 2017, Kansas researchers published results of a study in older adults with mild or moderate Alzheimer’s Disease. The 15 participants were fed a ketogenic diet supplemented with MCT oil for three months. All four subjects with moderate Alzheimer’s dropped out; the intervention was too burdensome for their caregivers. But 10 of 11 with mild Alzheimer’s stayed on the diet and experienced significant improvements on cognitive tests. However, a month after stopping the diet, those improvements were lost.32
- A 2020 systematic review of randomized controlled trials concluded that being in ketosis, either using a ketogenic diet, ketone supplements, or MCT supplements, “appears promising in improving both acute and long-term cognition among patients with AD/MCI (Alzheimer’s Disease or mild cognitive impairment).” They also noted a greater beneficial effect in those without an ApoE4 variant of the ApoE gene.33
A small family study of N=3
For four weeks in the winter of 2018, I helped my parents, both then-aged 92, do the keto diet to see if it would noticeably improve their brain health and cognitive functioning.
Before we started our experiment, I weighed them and measured their height, waist, leg, hip and arm circumferences. Neither one has ever been overweight; losing too much weight and becoming too frail were of concern. My mother was 5’2″ (157 cm) and 111 lbs (50 kg), with a BMI of 21. My father was 5’9” (175 cm) and 160 lbs (73 kg), with a BMI of 23.6. We ate three keto meals a day, with no fasting, and I kept their calories high to try to prevent weight loss.
My mother was not taking a single prescription medication — a rarity for a senior — so we did not need to worry about how the diet might affect drug interactions for her. My father was taking five medications: a diuretic and beta blocker for blood pressure and mild heart failure, a drug for a hypoactive thyroid, and warfarin and a baby aspirin for atrial fibrillation and stroke prevention. He was a doctor and professor of surgery in his career and he felt confident his medication levels would be fine and did not need adjusting during the experiment.
Before starting the keto diet, I separately gave each of my parents the Montreal Cognitive Assessment (MoCA) test. It is a validated 30-point, 15-minute test which family doctors can do in their office to identify patients with cognitive impairment. It includes tasks like drawing a clock face with the hands at a specific time, drawing a geometric shape, identifying four exotic animals in pictures, remembering five words without prompting, and subtracting sevens in sequence from a starting number, among other verbal, reasoning, and memory tests.
My father only had trouble with the delayed recall of four out of five words. He got a normal score of 26/30.
My mother on the MOCA struggled with a number of sections: putting the hands on the clock face for the right time, drawing the 3D geometric shape, naming the exotic animals, subtracting sevens, and listing all words she knew starting with F. But she had no problem with the attention and delayed recall of words. However, she scored lower than we expected, in the high teens.
Delicious meals, no hunger, no keto flu
For the next four weeks we followed the Diet Doctor ketogenic recipes for breakfast, lunch and dinner. Eggs — fried, scrambled, poached, baked — and either bacon or sausage were typical breakfast items, usually with avocado and cherry tomatoes on the side. For variety, some days we tried the various recipes for keto pancakes, always served with whipping cream and blueberries. The pancake recipe using cottage cheese was the hands-down favourite. Morning coffee and afternoon tea had full-fat cream and a spoonful of coconut oil.
A typical lunch was a salad with homemade soup (such as vegetables and meat in a bone broth base, or mushroom soup in a full-fat cream sauce), often with a cheese plate and keto seed crackers.
Dinner was usually a simple protein — a piece of fish (adding capers to the yummy baked salmon with lemon) or meat (roast chicken, roast beef) — with a salad and vegetables (always with butter or a cheese sauce.) The “crack slaw” stuffed cabbage casserole and the sausage, cauliflower and broccoli casserole were also favourites — with plenty of leftovers for lunches. Berries and whipping cream, with a square of 85% chocolate, was the typical evening dessert.
“The food was delicious, and we never felt hungry,” said my mother.
We had removed their typical meal items such as bread, potatoes, rice and a nightly high-carb dessert. The only thing Dad missed was the occasional piece of Mom’s apple pie, but when we made the low-carb baked apple dessert that hankering was easily met.
Ketostix showed that they both entered light ketosis within two days, with no keto flu nor any other side effects. Every few days I would measure the more accurate blood ketones against the ketostix results.
While the three of us were eating exactly the same diet and almost identical portion sizes, our ketone readings were quite different from each other.
At that time I’d been eating a keto diet for three years and my blood markers showed my blood readings ranging from 1.9 mmol/L to as high as 3.3 mmol/L. Mom’s ketones ranged from 0.7 to 1.3 mmol/L. Dad’s ranged from 0.6 to 0.9 mmol/L, never higher.
Cunnane’s group has published findings showing there is no difference in the ability of younger vs. older adults to make ketones.34 “The different ketone response of different people is well-known and is hard to account for,” he told me.
My weight stayed stable the whole time at 136 pounds (62 kilos). Mom dropped 3 pounds (1 kilos) and Dad dropped 5 pounds (2 kilos) in the first five days — and stayed at the lower weight. I was worried that if they continued to lose weight, we would have to stop the experiment. But after that first week, they lost no more.
I added butter, whipping cream, and coconut oil to absolutely everything, which is maybe why my ketone readings were so high but my weight stayed steady. I wasn’t burning any of my own body fat and the ketones in my blood reflected all the fat I was eating.
What did the cognitive tests show?
After two weeks of ketosis, we did another version of the MoCA test (same basic style, different questions.) Dad’s score went up by 3 points to 29/30. (He admits to practicing memorizing a list of words in the interim, but that mental motivation and stimulation is fair game.) Mom went up by five points to 22/30 — a significant improvement. We felt those were impressive results.
They reported, however, that physically they didn’t feel any different. Ketosis did not give them the energy spurt and subjective feelings of mental clarity that many others describe. But they liked the food all the same.
Two weeks later — after a total of four weeks of keto eating — we did another version of the test one more time. Dad was still 29/30 — great for a man of 92. Mom for the first time felt anxious and scared of the test. I tried to make it comfortable and light for her, just an interesting family experiment. But we both knew that her results really mattered to her. She slipped two points to 20/30, still higher than her original score pre-keto, but not as high as we had hoped.
My parents continued the keto diet for a total of about two months, but then gradually resumed their former pattern of eating, especially as caregivers came into their home to help make their meals.
My mother was diagnosed with Alzheimer’s Disease in early in 2020 and died in November 2021, age 95. My father remained cognitively bright and competent until his death in June 2022 at age 96. Both felt at the time that their short keto experiment was a worthwhile test, but was difficult to maintain on their own without my cooking help.
It may be impossible to turn back the hands of time, but we felt a sense of control and comfort by trying to get more ketones to their brains at least for the short term.
[/text_left]
Top posts and guides about keto
Top posts by Anne Mullens
Top keto videos
Alzheimer’s




The ketogenic diet for Alzheimer’s prevention and treatment: Can it help? - the evidence
This guide is written by Anne Mullens and was last updated on June 19, 2025. It was medically reviewed by Dr. Michael Tamber, MD on January 26, 2022.
The guide contains scientific references. You can find these in the notes throughout the text, and click the links to read the peer-reviewed scientific papers. When appropriate we include a grading of the strength of the evidence, with a link to our policy on this. Our evidence-based guides are updated at least once per year to reflect and reference the latest science on the topic.
All our evidence-based health guides are written or reviewed by medical doctors who are experts on the topic. To stay unbiased we show no ads, sell no physical products, and take no money from the industry. We're fully funded by the people, via an optional membership. Most information at Diet Doctor is free forever.
Read more about our policies and work with evidence-based guides, nutritional controversies, our editorial team, and our medical review board.
Should you find any inaccuracy in this guide, please email andreas@dietdoctor.com.
Alzheimers Dementia 2011: National estimates of the prevalence of Alzheimer’s Disease in the United States [overview article; ungraded]
Alzheimers.org: 2019 Alzheimer’s Disease facts and figures [overview article; ungraded] ↩
Progress in Neurobiology 2014: Is Alzheimer’s Disease related to metabolic syndrome? A Wnt signaling conundrum [overview article; ungraded]
Journal of Medicine and Life 2019: Possibilities of dementia prevention – it is never too early to start [overview article; ungraded] ↩
Diabetes Research and Clinical Practice 2018: Effect of dietary carbohydrate restriction on glycemic control in adults with diabetes: A systematic review and meta-analysis [strong evidence]
Obesity Reviews 2016: Impact of low‐carbohydrate diet on body composition: meta‐analysis of randomized controlled studies [strong evidence]
BMJ Open Diabetes Research and Care 2017: Systematic review and meta-analysis of dietary carbohydrate restriction in patients with type 2 diabetes [strong evidence]
Journal of Medicinal Food 2011: A pilot study of the Spanish ketogenic Mediterranean diet: an effective therapy for the metabolic syndrome [non-randomized, non-controlled study; weak evidence] ↩
Annals of Neurology 2010: Dementia incidence continues to increase with age in the oldest old: the 90+ study [longitudinal study; weak evidence] ↩
Alzheimer’s & Dementia: Translational Research & Clinical Interventions 2017: Alzheimer’s Disease drug development pipeline: 2017 [overview article; ungraded] ↩
Expert Opinion on Investigational Drugs 2017: Why do trials for Alzheimer’s Disease drugs keep failing? A discontinued drug perspective for 2010-2015 [overview article; ungraded] ↩
Archives of Gerontology and Geriatrics 2017: Concern about developing Alzheimer’s Disease or dementia and intention to be screened: an analysis of national survey data [descriptive study; ungraded]
European Journal of Aging 2012: Dementia worry: a psychological examination of an unexplored phenomenon [overview article; ungraded] ↩
Although the brain always needs some glucose, researchers have shown that during extended fasting or strict ketogenic eating, ketones can be used to meet up to 70% of the brain’s energy requirement:
Journal of Clinical Investigations 1967: Brain metabolism during fasting. [nonrandomized study, weak evidence]
Critical Care 2011: Clinical review: Ketones and brain injury. [overview article; ungraded]
Journal of Cerebral Blood flow and Metabolism 2017: Inverse relationship between brain glucose and ketone metabolism in adults during short-term moderate dietary ketosis: A dual tracer quantitative positron emission tomography study [nonrandomized study, weak evidence]
↩Frontiers in Endocrinology 2018: Unraveling the regulation of hepatic gluconeogenesis [overview article; ungraded] ↩
Epilepsia 2018: Effect of modified Atkins diet in adults with drug-resistant focal epilepsy: a randomized controlled trial [moderate evidence]
Acta Neurologica Scandinavica 2017: A randomized controlled trial of the ketogenic diet in refracatory childhood epilepsy [moderate evidence]
Epilepsy Research 2016: Evaluation of a simplified modified Atkins diet for use by parents with low levels of literacy in children with refractory epilepsy: a randomized controlled trial [moderate evidence] ↩
Frontiers in Pharmacology 2012: The ketogenic diet as a treatment paradigm for diverse neurological disorders [overview article; ungraded] ↩
Frontiers in Psychiatry 2017: The current status of the ketogenic diet in psychiatry
[overview article; ungraded] ↩Neurochemistry International 2018: Neuroketotherapeutics: a modern review of a century-old therapy [overview article; ungraded] ↩
Proceedings of the National Academy of Science U.S.A 2020: Diet modulates brain network stability, a biomarker for brain aging, in young adults [nonrandomized study, weak evidence] ↩
Diet Doctor will not benefit from your purchases. We do not show ads, use any affiliate links, sell products or take money from industry. Instead we’re funded by the people, via our optional membership. Learn more ↩
European neuropsychopharmacology 2014: Type 3 diabetes is sporadic Alzheimer׳s Disease: mini-review [overview article; ungraded] ↩
Frontiers in Neuroscience 2018: Alzheimer’s Disease and type 2 diabetes: a critical assessment of the shared pathological traits [overview article; ungraded] ↩
Diabetes 2004: Increased risk of type 2 diabetes in Alzheimer disease [observational study; very weak evidence] ↩
Alzheimer’s Dementia 2019: Evidence for brain glucose dysregulation in Alzheimer’s Disease [observational study; very weak evidence] ↩
Archives of Neurology 2011: Insulin resistance and Alzheimer-like reductions in regional cerebral glucose metabolism for cognitively normal adults with prediabetes or early type 2 diabetes [observational study; weak evidence]
Nutrition 2011: Brain fuel metabolism, aging, and Alzheimer’s Disease[overview article; ungraded]
↩PCOS is a reproductive metabolic disorder in which insulin resistance is a factor — and for which a low-carb or keto diet may be beneficial.
PLoS One 2010: Regional brain glucose hypometabolism in young women with polycystic ovary syndrome: possible link to mild insulin resistance [case-control study; very weak evidence] ↩
Archives of Neurology 1983: The fluorodeoxyglucose 18F scan in Alzheimer’s Disease and multi-infarct dementia [observational study; weak evidence]
In fact, some scientists propose using glucose metabolism as a surrogate marker for Alzheimer’s Disease
Alzheimer’s and Dementia 2020: Influence of cerebral glucose metabolic rate on cognitive function in Alzheimer’s subjects [nonrandomized study, weak evidence]
↩Journal of Alzheimer’s Disease 2015: Lower brain 18F-fluorodeoxyglucose uptake but normal 11C-acetoacetate metabolism in mild Alzheimer’s Disease dementia [case-control study; very weak evidence]
Experimental gerontology 2018: A cross-sectional comparison of brain glucose and ketone metabolism in cognitively healthy older adults, mild cognitive impairment and early Alzheimer’s Disease [case-control study; very weak evidence] ↩
Annals of the New York Academy of Sciences 2016: Can ketones compensate for deteriorating brain glucose uptake during aging? Implications for the risk and treatment of Alzheimer’s Disease [overview article; ungraded] ↩
Alzheimer’s Research and Therapy 2021: Randomized crossover trial of a modified ketogenic diet in Alzheimer’s Disease[moderate evidence] ↩
Neurobiology of Aging 2012: Dietary ketosis enhances memory in mild cognitive impairment [randomized trial; moderate evidence] ↩
Journal of Alzheimer’s Disease 2018: Ketogenic medium chain triglycerides increase brain energy metabolism in Alzheimer’s Disease [randomized trial; moderate evidence] ↩
Psychopharmacology 2016: Effect of a ketogenic meal on cognitive function in elderly adults: potential for cognitive enhancement [non-controlled study; weak evidence] ↩
Neuroscience Letters 2019: Effects of a medium-chain triglyceride-based ketogenic formula on cognitive function in patients with mild-to-moderate Alzheimer’s Disease [controlled and non-controlled studies; weak evidence] ↩
Regarding this trial, Dr. Ede said, “While more studies are needed, this suggests that the diet performed as well or better in people with mild Alzheimer’s Disease than any of the currently available Alzheimer’s medicines. If a new drug intervention had achieved that degree of improvement, people would be jumping up and down with excitement.”
Alzheimer’s & Dementia 2017: Feasibility and efficacy data from a ketogenic diet intervention in Alzheimer’s Disease [non-controlled study; weak evidence] ↩
Advances in Nutrition 2020:
To Keto or Not to Keto? A Systematic Review of Randomized Controlled Trials Assessing the Effects of Ketogenic Therapy on Alzheimer Disease [systematic review of randomized trials; strong evidence] ↩The Journal of Nutrition, Health & Aging 2009: Metabolic response to a ketogenic breakfast in the healthy elderly [non-controlled study; weak evidence] ↩