My path to low carb

I don’t have a heroic personal story about conquering diabetes or obesity with a low-carb diet. Rather, my low-carb epiphany occurred because of a timely encounter with a single diabetic patient… and his breakfast tray of waffles and fruit. On the way, however, I battled a lifetime of bad dietary advice.
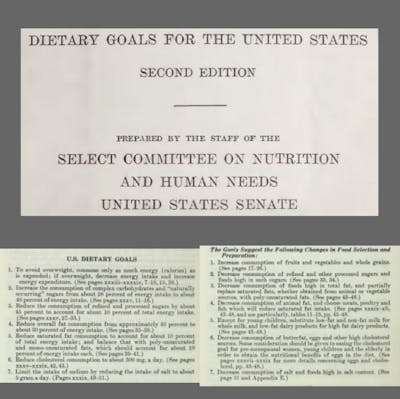
I, like nearly everyone else for the last 40 years, was a victim of the low-fat dogma that has largely contributed to the insulin resistance epidemic we are now facing. In fact, I was born less than 2 weeks before the release of the infamous McGovern report, Dietary Goals for the United States,in 1977, that demonized fat and cholesterol without legitimate science to support its tenets.
As a child, I recall all the attention being focused on the fat content of food, while there was substantially less concern about how much sugar I was consuming, except when it came to concerns about dental health. By no fault of their own, my parents provided their family with “heathy” low-fat meals, always buying lean ground beef, removing the skin from chicken, and buying the highly-marketed vegetable spreads in place of good old-fashioned butter.
Steering clear of fat, I recall consuming a large amount of Kool-Aid, lemonade, fruit juice, and soda. Gatorade, another sugary beverage, must also be okay to consume because it was designed for athletes who needed to replace their electrolytes (basically, nobody cared that adolescent boys drank it like it was going out of style, whether or not their electrolytes were truly depleted from physical activity).



Not knowing that carbs were really no better than sugar, I was a “carb junkie” as a kid. That’s what happens when you’re trying to avoid fat. I recall that one of my favorite after-school snacks was a couple pieces of bread slathered with the appalling vegetable spread, “I Can’t Believe It’s Not Butter”, and, for all I knew, eating bread was “healthy”. Low-fat – check. Multi-grain – check. Fiber – check. Polyunsaturated fats – check.
Battle with carbs
Fast-forward to my 1st year of medical school – I had put on the standard weight in college after consuming more than my share of pasta, grilled cheese sandwiches, and Mountain Dew in the buffet-style dining center, and now I’m living on my own and having to prepare my own meals. Out of convenience, given the time constraints of class and studying, I resorted to cheap, quick-fix meals like Tuna Helper dishes, frozen burritos, and spaghetti. I continued to gain weight during medical school on this carb-heavy diet, and I felt like continued weight gain was inevitable unless I invested serious time and effort into some endurance sport like running or biking.
Interestingly, I recall a time when I desperately wanted to lose weight for a trip to Las Vegas. I was aware of low-carb diets like the Atkins Diet at this time, but, with my conventional education, had always thought that it was ludicrous to advocate eating bacon rather than an apple, for example. Nonetheless, I embarked on a low-carb diet for about a week before my Vegas trip, coupled with a more dedicated effort in the gym, and I managed to “lose” several pounds of weight. That weight loss, however, didn’t last, as I resorted to my simple, carb-heavy diet as soon as I returned, and the weight (predictably) came back.
Nutrition education
One of my classes in my first year of medical school was Nutrition, coordinated by a professor in the Biochemistry department. Collectively, my medical school class had very little concern for the class, for it was pretty standard fare, touting the basics of the US Food Pyramid – promoting whole grains and demonizing saturated fats. Nutrition, to us, was a “soft science” and was a relatively small area of content compared to the enormous amount of material we were trying to learn.
Nutrition lectures were of so little priority to us that, when selecting a day to skip class to go snow-skiing, we chose to skip the day when there were multiple nutrition lectures scheduled, with no real fear of being able to catch up on the material covered. Not only did I really enjoy skiing that day, but also I spared myself a few hours of mundane lecture about the same old nutritional teachings that I had heard all along. I’m really quite glad that I went on that ski trip, and everybody passed the Nutrition course.
Throughout my medical training, I continued to recognize that the field of Nutrition was largely dismissed by the medical community – evident to me from my educators and from non-academic healthcare professionals. Physicians generally did not concern themselves with the impact of diet on their patients’ health. More often than not, physicians would simply defer any discussion of nutrition to dietitians, and nobody really expected physicians to be any more engaged than that in the discussion of nutrition. Sadly, that is still the case and largely explains why so little has changed in the past 40 years.
Eat less, move more
After years of a high-carb diet, I predictably gained weight, but felt a bit helpless as I was just too busy to work out when I was already sleep-deprived during medical school and residency. I recall during my 3rd year of residency, I made a concerted effort to eat “healthier”. Consistent with my conventionally trained vat of knowledge, that meant “low-fat”. Though I drank a can of Mountain Dew (46 g sugar per can) daily (my preferred vessel for caffeine), I thought I was doing myself a huge favor by eating low-fat salads every day for lunch. The salad, however, was inevitably paired with a bottle of Naked Juice – Blue Machine, weighing in at 40 g of carbs, 29 of which are simple sugar. “It’s fruit, I would tell myself” – a victim of great marketing.
Somehow, despite this obscene sugar load, I still managed to lose about 10 pounds (5 kg) over the course of a few months, perhaps testament to how metabolically “broken” I was at the time. If I could lose weight while consuming so much sugar (over 100 gm daily), I must have been eating a whole lot more carbs previously, as this sugar-loaded diet apparently was an improvement compared to my previous diet.
Calories In, Calories Out
Then I hit 30. Apparently turning 30 drew my attention to the fact that I had put on a fair amount of weight during medical school and residency. I found inspiration in the bodybuilding community and committed to losing the extra weight I had accumulated. I said “Good-bye” to Mountain Dew for good, and I cleaned up my diet to follow a 40/40/20 breakdown of carbs/protein/fat.
Influenced by the conventional wisdom of how to lose weight, I also busted my tail with exercise for several months: HIIT (High-Intensity Interval Training) workouts on an elliptical nearly every day and weight-lifting every-other-day. Ultimately, I did lose fat and put on muscle, with a net loss of about 30 pounds (14 kg), but I was exhausted. Worse yet, I was completely bored by my food – my meals were a predictable regimen of egg whites and oatmeal in the morning, then limited portions of baked chicken and sweet potato fries several times throughout the day, often with a salad at dinner.
Lesson learned – losing weight by the Calories In, Calories Out paradigm is painful and unsustainable.
My low-carb epiphany
Fast forward to a few years ago when I was encouraged to do a Performance Improvement project while working as a hospitalist and thus was on the lookout for some aspect of patient care that was in need of improvement. I can still picture the moment I walked into a patient’s room one morning after reviewing his elevated glucoses from the day before in the range of 250-300 mg/dl (13.9-16.7 mmol/L), and there before him sat a tray with remnants of his “Diabetic Diet” breakfast – a Belgian-style waffle that filled a standard plate, maple syrup, and a bowl of fruit, similar to this image:



Sure is a lot of carbs, I thought. Did we really allow him to eat so many carbs in one meal on a diabetic diet? Why are my patients allowed to eat so many carbs? Waffles?!? with syrup?!? I’m struggling to control my patients’ glucose, and somebody’s feeding them waffles?!?
Eureka! I had found my project. This discovery was total nonsense to me. In this poignant moment, I knew immediately that I had a large task on my hands.
The same thing had been happening at all the other hospitals I had worked at previously, and yet I had never really appreciated the absurdity of the situation. Basically, I had previously taken a passive role when it came to nutrition and simply trusted that the dietitians had my patients’ best interests in mind. Regardless, I committed right then and there to learn all that I could about carbs and diabetes.
Exploring the low-carb literature
So began my foray into the low-carbohydrate world, realizing that the U.S. dietary guidelines were (and continue to be) dangerous and based more on political influence than science. I wish I had realized years ago what the supposed “diabetic diet” really entailed, rather than blindly trusting that there was a scientific basis for it. For one, where did the concept of “consistent carbohydrates” come from? Is there any evidence to support such an approach to managing diabetes? (Not particularly, and it’s really just intended to make insulin dosing easier.)
After scouring the literature, including hunting down the references cited in journal articles and consensus statements, I was profoundly disappointed to find that there is no good science to support the current dietary recommendations for managing diabetes. In short, my takeaway from the literature was this: The Standard American Diet (SAD) is so lousy that ANY change is associated with improvement in glycemic control. Just switching from simple carbs to complex carbs is enough to appreciate some benefits. But, that change is not enough. It’s essentially the equivalent of switching from smoking regular cigarettes to smoking low-tar cigarettes – less harmful, but still harmful.
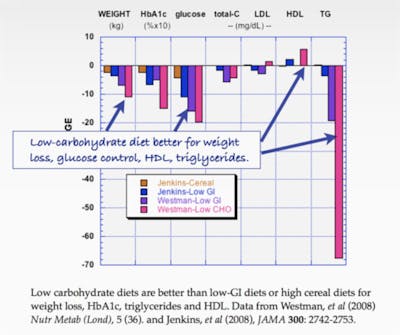
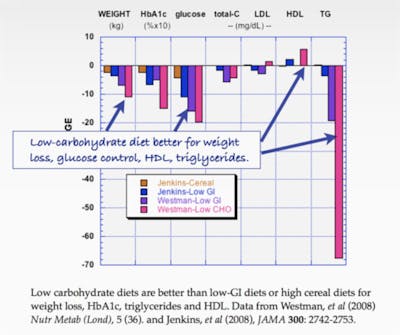
As I started exploring the literature on carbohydrate restriction in the management of diabetes, I realized that there was indeed a growing pocket of academics with the common sense to recommend carbohydrate restriction for a disorder of carbohydrate intolerance, i.e. type 2 diabetes mellitus. Much thanks to people like Dr. Eric Westman in North Carolina, Dr’s Nuttall and Gannon at the VA in Minneapolis, Minnesota, and Dr. Tim Noakes in South Africa, who all are working hard to perform quality scientific research demonstrating the efficacy of carbohydrate restriction in the management of type 2 diabetes.
I read their publications with the awe of someone experiencing a beautiful revelation for the first time and realized that carbohydrate restriction had the potential to make a big difference.
It only made sense – we treat gluten intolerance with elimination of gluten intake, and we treat lactose intolerance with elimination of lactose intake. Why, then, do we not tell carbohydrate-intolerant individuals (type 2 diabetics) to eliminate carbohydrate intake? That seems like the most basic of concepts to me. Still, despite my common-sense approach in the hospital, my initiative to restrict carbohydrate intake for those who suffer from diabetes has ruffled the feathers of more than one dietitian, to say the least.
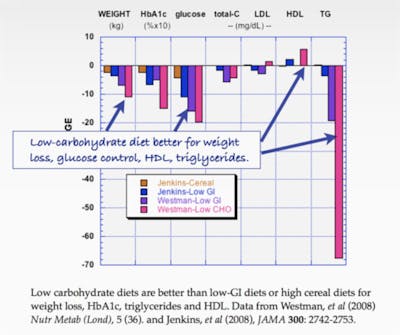
To me, there was indisputable evidence that a LCHF diet was also the best thing for my own health, as it has been demonstrated to provide favorable effects on all markers of the metabolic syndrome.
I had always been worried that I wouldn’t be able to control my weight in the future, since progressive weight gain appeared to be the norm in the general population. Furthermore, if I was going to recommend this dietary change to my acutely ill patients, I needed to test it out on myself first.
Since I started eating LCHF, I have, for the first time in my life, felt in control of my weight and my health. Aside from ongoing fat loss, I have appreciated numerous other benefits that are unmistakably attributed to eating low-carb, to be detailed in a later post.
Moving forward with LCHF
It was primarily the drive to improve the care of my patients that forced me to explore the science of nutrition and to appreciate the value of a low-carb, real-food lifestyle. Seeing the long-term, crippling effects of decades of poor dietary decisions was and continues to be a powerful reminder that food matters.
There’s no going back for me… I know that carbohydrate restriction is the right thing for my diabetic patients, as well as for those with other manifestations of insulin resistance. By entering medicine, I committed to a lifetime of working to improve the health of other people, and I now have a most powerful tool to transform lives. As I impart nutritional wisdom on my patients who suffer the consequences of several decades of bad nutritional advice, I’m still kicking myself for depriving myself of real food for so many years as I now enjoy with a low-carb, high-fat lifestyle. No more bread covered in vegetable oil spread for me, and no more waffles covered in syrup for my patients.
More
How to reverse type 2 diabetes