Metabolic Health and Nutrition Conference – part 3

I earlier this year attended a conference in Seattle, WA, (USA) titled “Metabolic Health and Nutrition Across the Life Span.” The headlining presenters were Dr. David Ludwig and Dr. Robert Lustig – both pediatric endocrinologists, researchers, authors, etc.
Though my notebook overflows with wisdom, practical tips, inspiration and what-if’s, I’d like to share some of the salient points that made this conference worth my time and effort to attend. If one wishes to dive deeper, there is far more information available in each of these presenters’ websites and publications.
Part 3: Reversing epidemics – exploring the utility of the ketogenic diet in reversing diabetes and applying functional medicine to reverse the epidemic of Alzheimer’s disease.
Want to reverse diabetes? Start by ignoring the guidelines! Metabolic disease: From management to reversal
Jeff Stanley, M.D.
1 in 7 adults in USA have type 2 diabetes, and the incidence is increasing steadily, along with the associated health care costs. The traditional teaching is that type 2 diabetes is chronic and irreversible.
The ACCORD trial sought to demonstrate that intensive glycemic control (primarily with the use of insulin) can reduce diabetes-related complications, however, there were noteworthy side effects:
- Compared to the subjects receiving standard treatment, subjects receiving the intensive treatment (insulin) gained more weight (~ 5 kg) and had higher mortality (causing a premature end to the study).
- Mediterranean – 6 RCTs looking at glycemic control in diabetes mellitus with variable results – 2 showed no difference, 2 showed that a low carb approach was superior to the traditional Mediterranean diet. Overall, it is probably a reasonable approach.
- DASH diet – of 8 studies cited, only 1 was RCT and didn’t show improvement in glucose.
- Plant-based diet – 3 studies, 1 was small RCT with 11 patients showing improvement. 1 showed decreased weight, but no decrease in glucose. 1 showed no decrease in glucose.
The common theme among the recommended diets for diabetes is low-fat, despite the guidelines explicitly recommending an “individualized” dietary approach, with no particular macronutrient breakdown.
Low-carb diet was not acknowledged as an acceptable approach in the 2018 guidelines, however, the 2013 guidelines looked at the low carb diet. 11 studies were reviewed – 7 of which showed a clear advantage for low carb. Four showed no difference in glycemic control, but two of those showed greater medication reduction (no difference in glucose, because on less medication) One study combined patients with and without diabetes, and the diabetic patients did have significant reduction in glucose. One study analyzed a combined low-fat and low-carb diet – that results in a high-protein diet, which is not well tolerated by many people.
There is a double standard when it comes to recommending dietary patterns for diabetes – despite the fact that there is no long-term evidence for the DASH diet (cited a study lasting only 8 weeks) for diabetes, they voice the need for caution regarding long-term use of a low-carb diet.
There is, however, good evidence from multiple RCT’s for a low-carb or ketogenic diet in improving glycemic control, and the concerns expressed about cardiovascular health have not been realized.
Multiple RCT’s show improved glucoses and/or reduction in diabetes medications on a low-carb/ketogenic diet, even without calorie restriction.
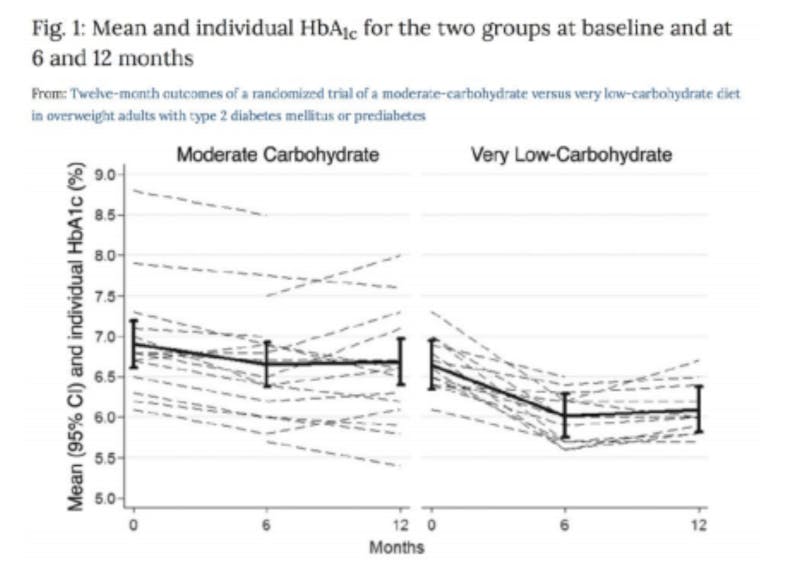
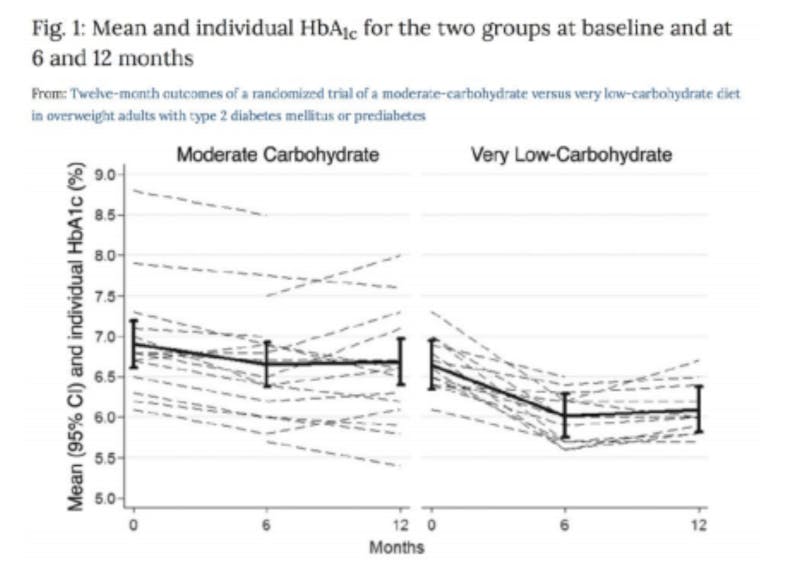
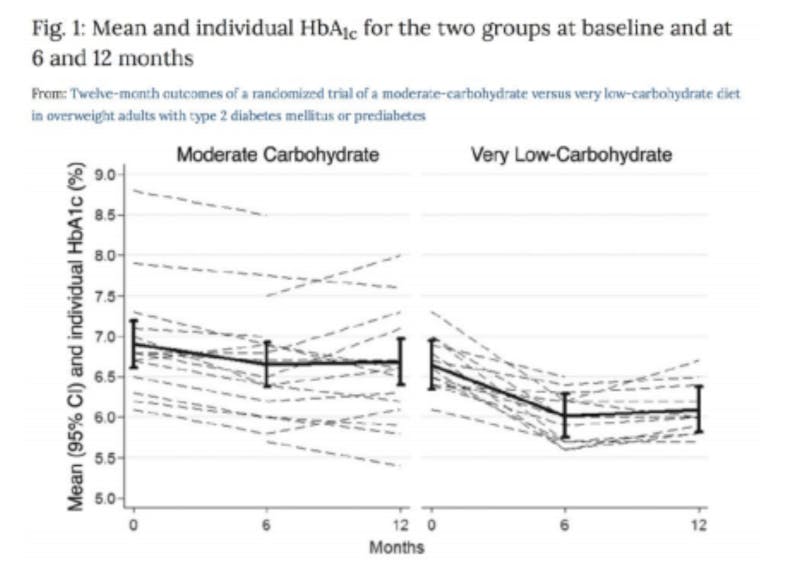
Dr. Sarah Hallberg is directing ongoing research on a low carb/ketogenic diet for diabetes at Indiana University Health. 400 patients treated “live” in clinic with group meetings, 400 patients treated “virtually” via internet portal, and 87 control patients receiving standard of care. Study has generated three papers so far.
Some of the results at one year are summarized in the below figure.
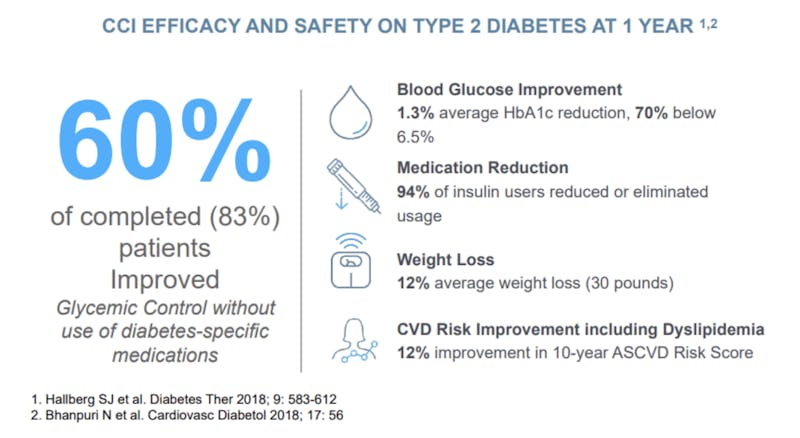
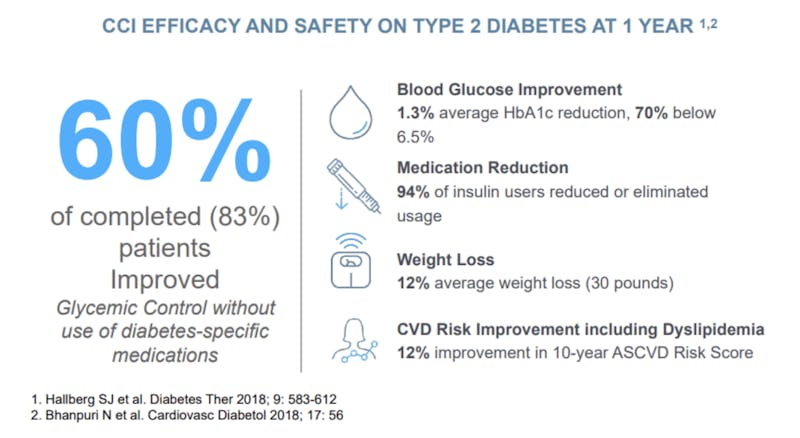
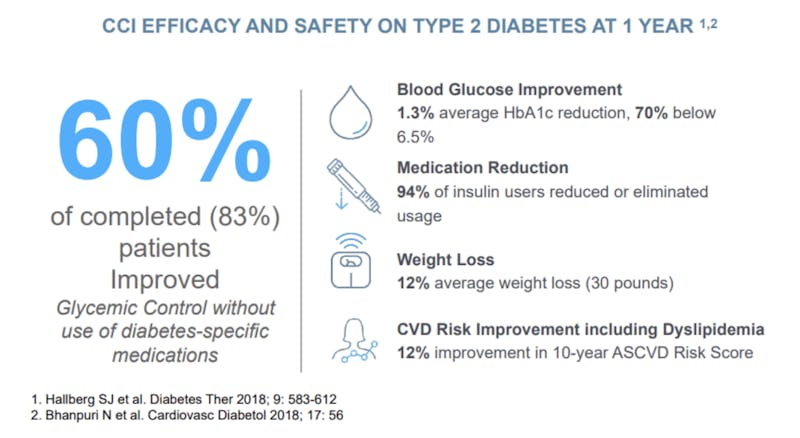
Patients remain engaged in the electronic app (83% after 1 year), experience progressive and sustained weight loss, and are able to sustain nutritional ketosis for many months continuously without ill effect.
In regards to cardiovascular risk factors, 25 of 29 factors improved in a “favorable” direction. Though LDL increased by 10% (traditionally considered unfavorable), the LDL pattern became more “fluffy” [Pattern A] (favorable).
Beta-hydroxybutyrate (the predominant ketone present in nutritional ketosis) is an efficient fuel source for the brain, heart, and skeletal muscle.
Conclusions:
- Low-carb and ketogenic diets are not “fads”.
- There is ample evidence to support their safety and efficacy in managing type 2 diabetes.
- Nutrition guidelines need to reflect the best evidence and be consistent in their assessment of varying dietary patterns.
- Patients deserve choices and support from their physicians and providers.
Pediatric Gerontology – No, I’m not kidding…
Dale Bredesen, M.D.
Dr. Bredesen started a lab 30 years ago and left clinical practice 25 years ago to focus on what’s driving the neurodegenerative process of Alzheimer’s disease.
Neurodegenerative disease is arguably the area of greatest failure in medicine. There have been billions of dollars spent on over 400 failed clinical trials, and the only “successes” (e.g. donepezil, trade name Aricept) fail to alter cognitive decline.
Alzheimer’s disease, thought of as a disease of the elderly, is increasingly common in younger ages, e.g. 50 year-olds.
In health care, we treat without knowing the cause of dementia. There has been a search for “the cause” of Alzheimer’s, but it is becoming evident that there is actually a multitude of factors.
Amyloid is a mediator – not the root cause.
There are dozens and dozens of things that contribute to the response of your brain that we ultimately call Alzheimer’s.
Current standard: 1 cause -> 1 disease -> 1 treatment (monotherapy, ineffective)
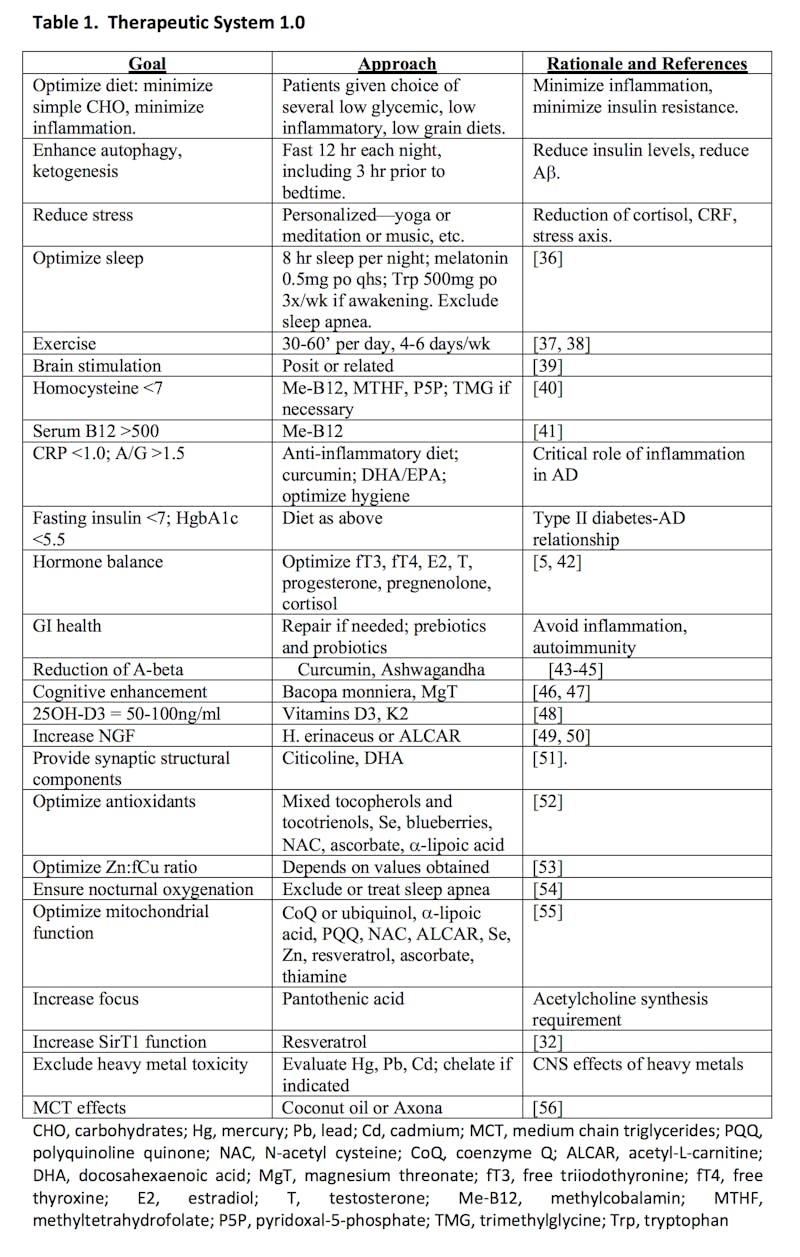
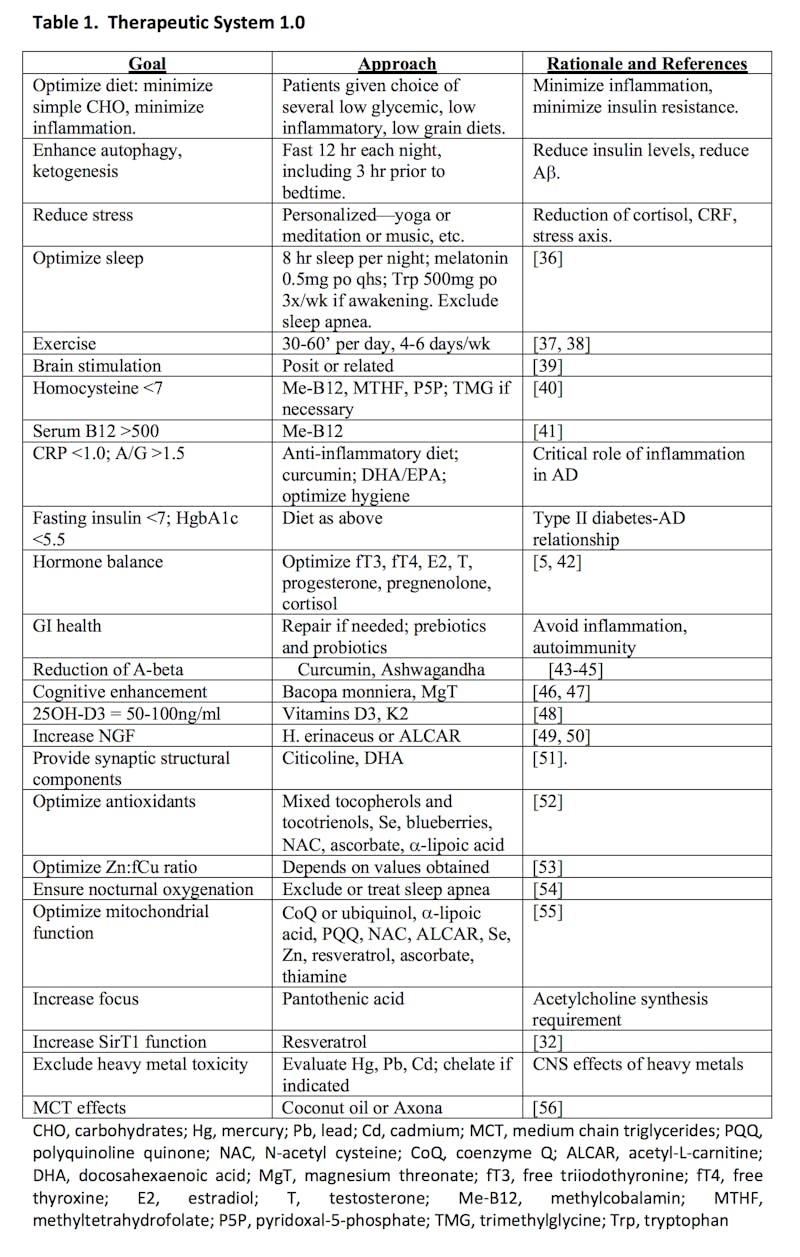
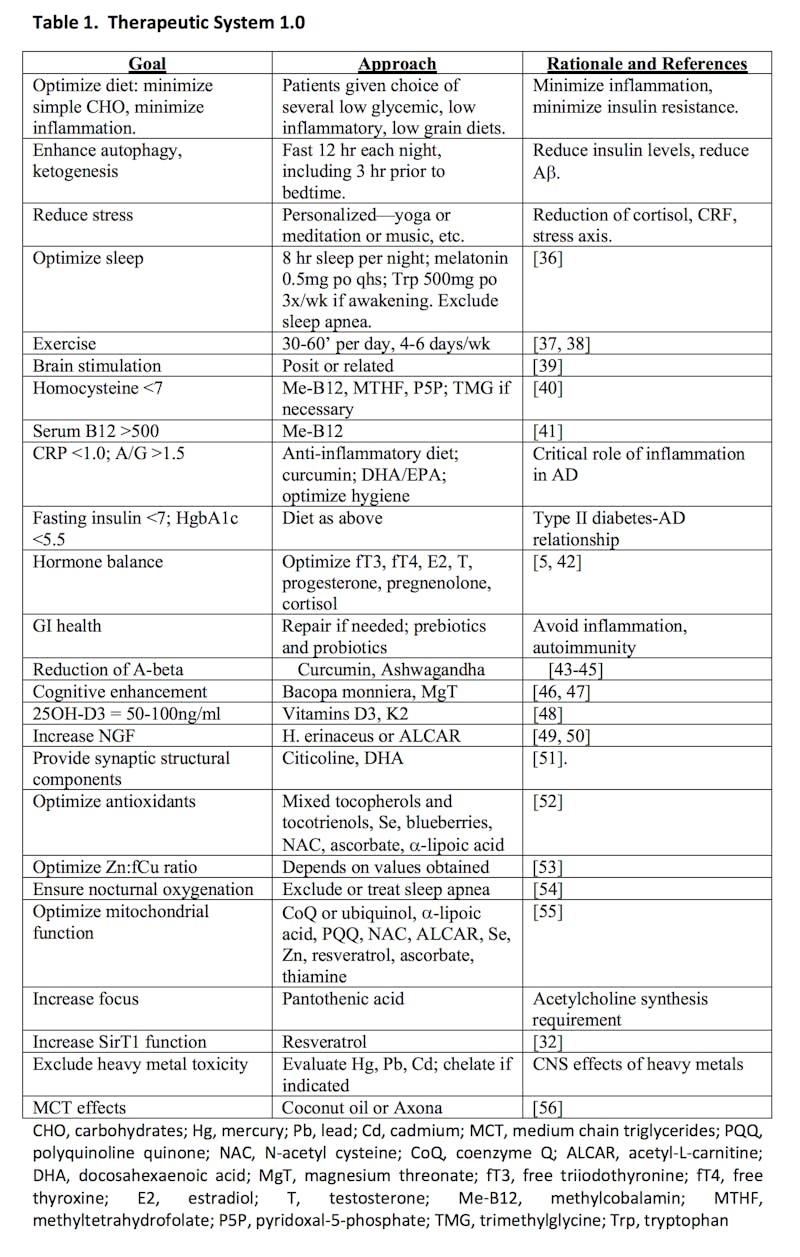
Research findings: 36 contributors -> 6 subtypes -> many treatments (personalized programs)
Alzheimer’s Disease is a result of a protective response to metabolic and toxic disturbances: inflammation, insulin resistance/glycotoxicity, nutrient withdrawal, and specific toxins.
By use of Dr. Bredesen’s ReCODE (Reversal of Cognitive Decline) protocol, cognitive decline in Alzheimer’s is reversible. This program should be applicable to other chronic diseases, as well.
Referring to Alzheimer’s as “type 3 diabetes” is an oversimplification. Insulin resistance and glycotoxicity contribute to the inflammatory type of Alzheimer’s, and alteration of insulin signaling contributes to the atrophic type of Alzheimer’s. Thus, a subset of Alzheimer’s could be thought of as “type 3 diabetes”.
His lab hasn’t seen a single patient without at least 10 factors known to contribute to Alzheimer’s.
This research paper from 2014 describes the treatment system, as well as the stories of three patients participating in his lab’s protocol. Several more patient stories are described in this 2016 paper.