Sinking our teeth into the carnivore diet: what’s known, what’s not
T-bones for breakfast, ground round for lunch, rib eyes for dinner. Does this sound like your dream menu — or your worst nightmare? Is a diet consisting of only animal products a simple, healing way to eat or an overly restrictive regimen that borders on an eating disorder?
A carnivore diet contains animal products only. It is plant-free. In its most extreme form, it includes only meat and water.
Read on to learn more about the zero-carb, carnivore way of eating. And find out the results — positive and negative — I experienced when I tried the diet for 30 days.
Why explore carnivore eating?
At Diet Doctor we do our best to examine the best scientific evidence available to support safe and sensible dietary decisions to help you improve your health.
Some burgeoning dietary regimens, however, lack high-quality evidence either for or against their use. For the carnivore diet, there are a growing number of anecdotes, a wide range of expert opinions, and some interesting evolutionary theories. However, very few research studies exist around carnivory.
Should we ignore the growing popularity of carnivore eating because of these scientific limitations and pretend it doesn’t exist? Or should we acknowledge it and discuss what is known and not known about its potential benefits and harms? We have chosen the latter approach but strongly stress that much more experimental research needs to be done.
What to eat on the carnivore diet
So, what do you actually eat on the diet? Also called a zero-carb diet or animal-sourced foods (ASF) diet, the carnivore diet typically consists of 100% animal foods — meat, fish, eggs, high-fat dairy products, and animal fats. Some adherents eat only meat, salt, and water. Others allow for exceptions like coffee, tea, and small amounts of spices used in cooking, if tolerated.
According to a survey of 170 participants who had been following a carnivore
diet for at least six months, the exact composition of the diet may differ widely
among individuals due to food preferences or other considerations. Beef was the
most common food consumed across the group, but a wide variety of animal foods was reported.1
The carnivore diet has been getting a lot of attention lately. There are Reddit forums with thousands of members, many Facebook groups, numerous articles in mainstream media, podcasts and hundreds of YouTube videos.
However, is a trial of the diet right for you?
Videos about meat
At Diet Doctor we recommend above-ground vegetables in our low-carb and keto guides and recipes. This suits most people very well because such vegetables are very low in carbs and contain a lot of fibre, nutrients, and trace minerals. They can also be filling. One can generally eat a few servings of kale, broccoli, cauliflower, Brussels sprouts, zucchini, and other veggies without exceeding 20 grams of net carbs a day. Moreover, eating a mixture of non-starchy vegetables with animal products like meat and cheese provides good dietary variety, which can make low-carb eating more interesting and sustainable for the long term.2
Not everyone, however, achieves complete success on a low-carb ketogenic diet that is rich in vegetables. According to comments gleaned from various carnivory websites, Facebook groups, and discussion forums, some people tried a keto diet first but were dissatisfied with their results, prompting the trial of carnivory. “By and large, most people doing the carnivore diet have some persistent health issue that the keto diet did not completely fix, such as not enough weight loss, a mental health condition, an autoimmune condition, or uncontrolled cravings,” says Dr. Paul Mabry, a zero-carb US family doctor who blogs at Born to Eat Meat and manages a Facebook group, Zero Carb Doc, which now has more than 8,500 members. Dr. Mabry says he was “a total sugar addict” who at first did well on a keto diet that included lots of vegetables. He lost 50 pounds on keto, but his weight stalled at 230 pounds — which was about 50 pounds above his ideal weight. Plus, his hand eczema, cravings and tendency to overeat continued. “Even the tiniest amount of carbs can start my cravings and binging,” said Dr. Mabry. In 2015 he began a carnivore diet, eating almost 80% fat and 20% protein. His weight dropped, his hand rashes cleared, and his cravings stopped. He has now maintained a weight of 180 pounds with no issues. “I don’t think everyone needs to eat a zero-carb diet. But if you are like me, someone who is severely metabolically damaged from a lifetime of sugar addiction, I think it can help,” he says, calling it a total abstinence approach to carbs. Australian Jane Jordan, a former nurse, did the keto diet for seven years, with good results. She lost weight, normalized her blood sugar and blood pressure, and eliminated her migraines and IBS. In spring 2018, when Jordan was diagnosed with early-stage glaucoma, a condition that runs in her family, she found some posts that zero-carb might help her eyesight.3 Recent research has suggested that Vitamin B3, known as nicotinamide, may potentially be an effective preventive agent or treatment for glaucoma.4 The foods highest in nicotinamide include meat, poultry and seafood. “Why not try it? I had nothing to lose,” said Jordan. After seven months of the carnivore diet, a retest of her eyes by her optometrist in October 2018 found no evidence of the disease. “I am convinced that it was the zero-carb diet that reversed it,” she says.5
There are currently no research trials examining the carnivore diet for glaucoma. But stories of health improvement can even be found as far back as 1799, where a case report was published describing a meat-only diet being used in conjunction with other therapies to “permanently cure” a case of type 2 diabetes (although it would more likely be accurately described as “remission” or “management”).6
It is clear, however, that success is not guaranteed for all on the diet. Other people in Facebook groups and discussion forums have complained of weight gain, bloating, digestive upset, increased body odor, increased acne, increased tartar on teeth, and other unwanted or lackluster results after adopting a zero-carb diet.7
Popular podcast host Joe Rogan publically commented on his “explosive diarrhea,” but noted this self-resolved after a couple weeks. Non-peer reviewed surveys from Dr. Shawn Baker and Amber O’Hearn report infrequent side effects and mostly beneficial findings.8
Among low-carb experts, the carnivore diet is controversial. Low-carb neuroscientist Rhonda Patrick, PhD, is concerned about the potential for negative gut microbiome changes and the risk of micronutrient deficiencies. “What is attracting someone to try such a restrictive diet without any published studies or long-term evidence? Why would you do it?” she said in an October 2018 podcast with Joe Rogan. She said the most common reason seems to be trying to influence ongoing autoimmune conditions. Psychiatrist Dr. Georgia Ede supports a trial of the diet. In her popular Diagnosis Diet blog and in this Diet Doctor video , she explores whether vegetables are truly necessary for health. While there are ample data reporting health benefits from eating vegetables, the question remains if someone can maintain good health long-term while completely avoiding vegetables. She told participants at the 2018 Low-Carb San Diego conference that she was currently trying a carnivore diet herself and, so far, was experiencing positive results, such as improved sleep, steady mood and resolution to her migraines and night-time leg cramps. Dr. Ted Naiman says he has now had many patients who have done 30-, 60-, and 90-day trials of the carnivore diet, with generally good results and normal labs. However, he has been finding that longer term, the diet may be more concerning. “I’ve now had a small handful of patients who were doing this longer than six months who have reported vague fatigue. The lab workup in these people is usually normal except for very low folate levels, below the normal range.” (Folate, or vitamin B9, is an essential vitamin found in high amounts in green vegetables, egg yolks, organ meats, avocado and legumes. Here is a list of food folate sources.) Dr. Steve Phinney is concerned about potential deficiencies in sodium, magnesium, and potassium in those who follow the carnivore diet.9
Dr. Jason Fung says, “There is little research evidence around it. But if people are doing well on it, I don’t have a problem with it. And if micronutrients are an issue, you can always take a daily vitamin.” Other low-carb experts who were approached for their opinion for this story decided to pass: “There are no long-term studies. I’d rather not comment,” was a common response. Most mainstream dietary experts, who generally don’t support low-carb ketogenic eating, are alarmed. They call the carnivore diet extreme, insane, and a bad idea. Despite the controversy, some high-profile individuals are sharing how a carnivore diet helped resolve their intractable problems, especially mental illness and serious autoimmune conditions. One of the most prominent and dramatic stories is of Canadian Mikhaila Peterson, who had juvenile rheumatoid arthritis that was so severe she’d had three joint replacements (a hip and two ankles) before age 17. She also had extreme fatigue, anxiety, and depression. In 2015 she began eliminating foods to see if a specific food was contributing to her autoimmune issues. She ended up eating just beef, salt and water — and all her symptoms disappeared. Peterson’s father is the controversial University of Toronto psychologist Jordan Peterson, PhD, the bestselling author of 12 Rules For Life. Peterson witnessed his daughter’s improvements, adopted the same diet, and has said it caused his long-term depression to lift. Both Mikhaila and Jordan’s stories have been featured on Diet Doctor. Other high-profile advocates include orthopedic surgeon Dr. Shawn Baker, Kelly Hogan who blogs at My Zero Carb Life, and Esmée La Fleur who runs the ZeroCarbZen website, where she interviews other carnivores about how the diet has impacted their health. Meat Rx, Dr. Baker’s website, collects hundreds of testimonials of personal health transformations. Just Meat, curated by bitcoin entrepreneur Michael Goldstein, has a large collection of articles, historic documents, archeological studies, and other carnivory links. Included at ZeroCarbZen are all the archives of the late Owsley Stanley, a.k.a “The Bear”, the former sound engineer (and LSD supplier) to the Grateful Dead. Stanley was a carnivore for some 50 years, and while the rock band happily took his drugs, they would not take his dietary advice. His story is fascinating reading. Some of the most scientific and nuanced writing on the carnivore diet is being done by Amber O’Hearn, who has a popular blog and website Mostly Fat. A computational mathematician, O’Hearn has been a carnivore for more than a decade and says she will stay on it for life, because it is the only way of eating she has found that controls her bipolar disorder. She speaks at many low-carb conferences, and even hosted her own carnivore conference in 2019. Her full-length podcast is available on the member side of Diet Doctor. “I don’t advocate eating a carnivore diet for no reason at all,” O’Hearn says. “If you can eat a more varied low-carb diet with good results, why wouldn’t you?” But she also rejects the dominant, unchallenged view that humans simply must eat vegetables for health and that pure carnivory is physiologically implausible. Although research regarding plant-free diets is scarce, and there are no randomized controlled trials, there are some publications on the topic.10 Amber O’Hearn, for example, published a paper stating that the diet can meet all micronutrient needs, including Vitamin C.11
A case series published in December of 2020 reported five out of six subjects starting a carnivore diet resolved their small intestine bacterial overgrowth (SIBO).12
A paper on the effects of a Paleolithic Ketogenic Diet (PKD) on serum magnesium levels showed normal levels in all but one person, and reports of leg cramping resolving on PKD (which can be triggered by magnesium deficiency).13
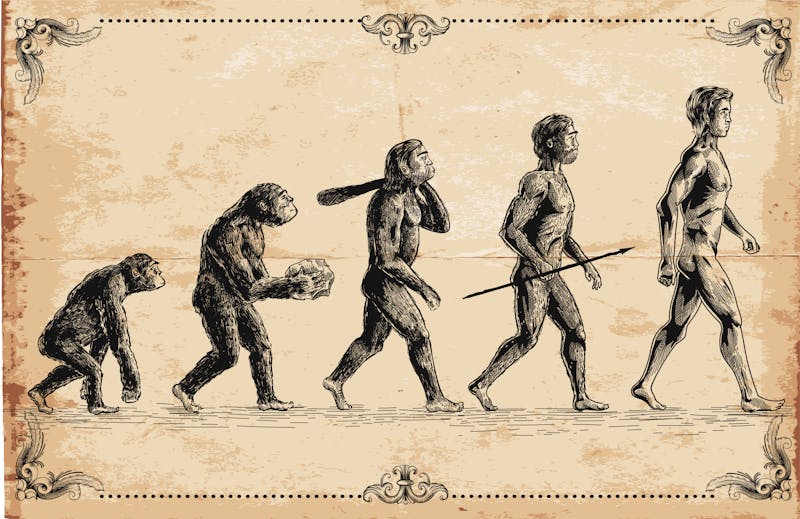
Finally, researchers from Harvard University, Dr. Belinda Lennerz and Dr. David Ludwig, published a study from over 2,000 individuals who self-reported their experience with a carnivore diet.14 The results were overwhelmingly positive with 93% improving or resolving obesity or overweight, 93% for hypertension, 98% for diabetes or insulin resistance, 97% for gastrointestinal symptoms, and 96% for psychiatric symptoms. Although the data quality are very low, given the high risk for selection bias with these self-reported outcomes, this study is an important first step toward larger, more rigorous investigations of a plant-free diet. So, do we need to eat plenty of plants for good health? What evidence exists that our human ancestors survived, and maybe even thrived, on a largely meat-based diet? Many of the people listed above draw upon common archeological, anthropological, and physiological sources to argue that humans evolved to be carnivores, and that fatty meat and organ meats are humans’ optimal diet. As hunter-gatherers, they say, people may have eaten plants, tubers, nuts, and seeds when meat was scarce — and gorged on summer fruit and berries to fatten up for winter — but such foods weren’t necessary to maintain health. Meat was.15
Here are some of the key points commonly used to argue that homo sapiens evolved to eat a diet mainly of meat and fat. While an increasing number of doctors are recommending the low-carb ketogenic diet to treat a variety of medical conditions, currently we are aware of only one medical clinic that is using the zero-carb, all animal-sourced diet as a therapy for a wide variety of serious conditions. That clinic is The International Center for Medical Nutritional Intervention (ICMNI) also popularly known as Paleomedicina in Zalaszentgrót, Hungary. The team, headed by research neuroscientist Dr. Zsófia Clemens and physician Dr. Csaba Tóth, uses its paleo-ketogenic diet therapeutic protocol to treat a wide array of autoimmune conditions, type 1 and type 2 diabetes, mental health conditions, and even cancer. Developed in 2010-2011, their protocol follows what the clinic believes early modern humans evolved to eat. The diet has a ratio of two parts animal fat to one part animal protein.28 Acceptable protein sources are fatty red meats and organ meats, preferably from pasture-raised animals. No nitrates, nitrites, or additives to meat are allowed. A very small amount of vegetables — mostly leafy greens — are allowed as long as they do not take people out of ketosis, but they are not deemed to be necessary. On the diet, eggs are at first eliminated but reintroduced after about six weeks to see whether they trigger any negative symptoms (for some, they do). The diet does not allow any dairy products, fruit, sugar, grains, starchy vegetables, or processed carbohydrates. Since 2013, the clinic has used their paleo-ketogenic diet to treat more than 10,000 patients, according to Dr. Tóth. They’ve published case studies of the reversal of Crohn’s disease, halting of the progression of type 1 diabetes, reversing a precancerous condition, and halting the growth of malignant cancer of the soft palate, the rectum, and the brain.29 Their groundbreaking but controversial work has been featured in a number of podcasts, articles and presentations. Their findings have not yet been reproduced by other researchers or studied in experimental trials. In an interview with Diet Doctor, Dr. Tóth described how he searched for years to find a way to cure his own health problems: type 2 diabetes, high blood pressure, severe eczema, and severe Crohn’s disease. He first found the paleo diet, which helped his conditions but did not cure them. It was only when he combined the paleo diet with the ketogenic diet that his health problems resolved.30“Moreover, every clinician in the clinic now eats this way, too,” he says. “We are convinced that this is the healthy way of eating.” Drs. Tóth and Clemens say their experience suggests that a key mechanism of the diet may be its positive impact on the function of the intestine, healing and reversing intestinal permeability, also sometimes called “leaky gut.” While in the past, mainstream medicine largely dismissed the theory of illnesses being linked to a leaky gut as being pseudo-science, recent research is confirming that a breakdown of the gut barrier can occur.31 Data from a number of academic institutions demonstrate that an increase in intestinal permeability is a common feature of a number of autoimmune and chronic disease conditions.32
A “healthy” intestine absorbs nutrients and energy for use by the body and is more likely to keep out microbes, antigens, and other potential disease-causing agents. The theory is that increased permeability allows unwanted substances to cross the intestinal barrier, triggering inflammation and a dysfunctional immune response.33 “If you have high intestinal permeability, then it is a high probability that all biological membranes are malfunctioning, such as the blood-brain barrier,” said Dr. Tóth.34 All of Paleomedicina patients undergo a test, called PEG400, to measure their level of intestinal permeability before and after starting the diet.35 Dr. Tóth said at Paleomedicina they have shown by repeating the test that their paleo-ketogenic diet can restore the gut wall to normal permeability within a few months.36
Don’t we need to eat vegetables and fibre to prevent colon cancer? Leading health institutions like the World Health Organization and the World Cancer Research Fund declare that red meat causes colorectal cancer and constantly urge us to eat less of it. Wouldn’t a meat-only diet increase the risk of developing cancer? Diet Doctor has an in-depth guide to red meat and another one on diet and cancer that discuss the weak evidence regarding red meat and cancer, as well as explore whether vegetables are protective. We direct you to those guides for a more detailed evaluation of meat and cancer risk. When Dr. Andreas Eenfeldt asked me to research and write this guide to carnivore eating, it became clear I should give the diet a try myself. I wasn’t so sure I wanted to. I love vegetables and salad. I have a big vegetable garden; tending it and eating its bounty is a source of joy. Plus, I’ve had no outstanding health complaints since adopting the ketogenic diet in 2015. I’m now happy with my weight; I’ve no auto-immune conditions nor mental health concerns; I’ve no trouble controlling carb cravings. In short, unlike many who try the carnivore diet, I didn’t have an overwhelming motivation — except this guide — to try this way of eating. In addition, I was reluctant to tell my family and friends I was eating only meat. It felt extreme. It did not lend itself to dinner parties, lunch dates with girlfriends, and other forms of socializing. I didn’t want to get lectures about the evils of meat or have friends think I’d developed an eating disorder. So, I embarked on a quiet trial, not telling anyone I was doing it. At first I thought I would just do a week, but I learned that would be too short to demonstrate anything. “It takes about 30 days to see appreciable differences from this diet and often longer, compared to a merely ketogenic one,” advises O’Hearn. The biggest surprises to me were how it nudged my stalled weight a few pounds, the calm gut and the improved skin. The most difficult was the tedium, the surges of body heat, the cravings, and my self-imposed feeling of social isolation from the diet. I thought often of Amber O’Hearn’s comment, “If you can eat a more varied low-carb diet with good results, why wouldn’t you?” That described me to a T (make that a T-bone!). I didn’t really need to do the diet, so the trade-offs were high. I had no concerning health reason to motivate me; it felt restrictive and limiting. I did not eat out with friends for a whole month. I was glad when my trial was over. I’m now back to eating a low-carb ketogenic diet with plenty of above-ground vegetables. I am happier making many of the delicious Diet Doctor recipes. That way of eating feels more enjoyable, balanced, and sustainable to me. That said, however, I understand better why those with severe or incurable conditions with poor therapeutic options might try carnivore eating. In the absence of any good scientific evidence pro or con, doing their own n=1 trial over a few months might determine if they are likely to experience any benefit. Short term, it is unlikely that it would do any harm. But as Dr. Naiman notes above, longer periods of zero-carb eating might cause health issues for some people. So it is important that anyone considering a trial should pay close attention to their individual responses. If there’s no improvement over weeks or a few months, it’s likely not helping, and people can feel satisfied returning to a more varied and less restrictive low-carb or ketogenic diet. Get delicious recipes, amazing meal plans, video courses, health guides, and weight loss advice from doctors, dietitians, and other experts.Why people turn to carnivory
Experts weigh in: some pro, some con— some alarmed
Testimonials, blogs and advocates bloom
Available Research on Carnivorous Diets
Threads of evidence from our ancient past
While none of these factors prove that in our modern age we would be better off limiting ourselves to a carnivore diet, they are key arguments used by carnivore diet proponents that humans evolved to rely heavily on animal-sourced foods.
Paleomedicina in Hungary: treating dire conditions with a zero-carb diet
The role of intestinal permeability
What about colon cancer?
N=1: My one-month trial
Calmer gut, lower body fat, more hot flashes
First, here is how I ate:
The results:
Start your FREE 7-day trial!
Sinking our teeth into the carnivore diet: what’s known, what’s not - the evidence
This guide is written by Anne Mullens and was last updated on June 19, 2025. It was medically reviewed by Dr. Bret Scher, MD on January 19, 2022 and Dr. Michael Tamber, MD on January 19, 2022.
The guide contains scientific references. You can find these in the notes throughout the text, and click the links to read the peer-reviewed scientific papers. When appropriate we include a grading of the strength of the evidence, with a link to our policy on this. Our evidence-based guides are updated at least once per year to reflect and reference the latest science on the topic.
All our evidence-based health guides are written or reviewed by medical doctors who are experts on the topic. To stay unbiased we show no ads, sell no physical products, and take no money from the industry. We're fully funded by the people, via an optional membership. Most information at Diet Doctor is free forever.
Read more about our policies and work with evidence-based guides, nutritional controversies, our editorial team, and our medical review board.
Should you find any inaccuracy in this guide, please email andreas@dietdoctor.com.
OSF Preprints 2020: Beliefs and Experiences of Individuals Following a Zero-Carb Diet: An Online Qualitative Study [nonrandomized study, weak evidence] ↩
This has been shown in both observational studies and trials lasting up to two years:
Diabetes, Metabolic Syndrome and Obesity 2019: Diet, diabetes status, and personal experiences of individuals with type 2 diabetes who self-selected and followed a low carbohydrate high fat diet [descriptive observational study; weak evidence]
Frontiers in Endocrinology 2019: Long-term effects of a novel continuous remote care intervention including nutritional ketosis for the management of type 2 diabetes: a 2-year non-randomized clinical trial [non-randomized study; weak evidence]
Annals of Internal Medicine 2010: Weight and metabolic outcomes after 2 years on a low-carbohydrate versus low-fat diet: a randomized trial [randomized trial; moderate evidence]
Diabetes, Obesity and Metabolism 2018: Effects of an energy-restricted low-carbohydrate, high unsaturated fat/low saturated fat diet versus a high-carbohydrate, low-fat diet in type 2 diabetes: A 2-year randomized clinical trial [randomized trial; moderate evidence] ↩
Journal of Glaucoma 2018 Glaucoma as a metabolic optic neuropathy: making the case for nicotinamide treatment in glaucoma [overview article; ungraded]
Science 2017: Vitamin B3 modulates mitochondrial vulnerability and prevents glaucoma in aged mice [mouse study; very weak evidence] ↩
While we can’t know if increased consumption of vitamin B3 helped, it’s also reasonable to suggest that adding a B3 supplement to her baseline diet would have been a reasonable experiment, as well.
The Medical and Physical Journal 1799: A Case of the Diabetes Mellitus, Which Terminated in a Complete, and, as Far as Can Be Judged from Apparent Circumstances, a Permanent Cure, by Medicines, Abstracting Oxygen from the System, and a Diet Consisting Totally of Animal Matter [Anecdotal report; very weak evidence] ↩
These data come from online surveys with a strong selection bias and are not published in peer reviewed journals.
Although there is no limitation to supplementing with salt or choosing potassium-rich foods like wild salmon and other fish. ↩
While some publications are in reputable, peer-reviewed journals, others are not peer-reviewed. ↩
Although the conclusion is that a more detailed study is needed (a common theme when discussing carnivore diets), the paper makes the case that carnivorous diets may be nutritionally adequate given the available evidence in existing research.
Current Opinions in Endocrinology, Diabetes, and Obesity 2020: Can a carnivore diet provide all essential nutrients?[overview article; ungraded] ↩
BMC Gastroenterology 2020: A Zero Carbohydrate, Carnivore Diet can Normalize Hydrogen Positive Small Intestinal Bacterial Overgrowth Lactulose Breath Tests: A Case Report [nonrandomized study, weak evidence] ↩
Although serum magnesium levels are not necessarily indicative of tissue magnesium levels, it is noted in the paper that low serum magnesium is not uncommon in those with diabetes or metabolic syndrome, which makes the lack of low serum magnesium notable given the makeup of the people studied. Further research looking at tissue levels of magnesium in people following PKD would help clarify the relevance of this result.
Journal of Evolution and Health: An Ancestral Health Society Publication 2018: The paleolithic ketogenic diet may ensure adequate serum magnesium levels [nonrandomized study, weak evidence] ↩
Current Developments in Nutrition 2021 Behavioral characteristics and self-reported health status among 2029 adults consuming a carnivore diet [non-randomized internet survey with self reported data, very weak evidence] ↩
Journal of Nutrition 2003: The critical role played by animal source foods in human (homo) evolution [overview article; ungraded] ↩
PLoS One 2011: Man the Fat Hunter: The Demise of Homo erectus and the Emergence of a New Hominin Lineage in the Middle Pleistocene (ca. 400 kyr) Levant [evolutionary study; ungraded] ↩
PLoS One 2015: The Evolution of Stomach Acidity and Its Relevance to the Human Microbiome [nonrandomized study, weak evidence] ↩
International Journal of Molecular Sciences 2018: The expensive-tissue hypothesis in vertebrates: gut microbiota effect, a review [review article; ungraded] ↩
Nature 2010: Evidence for stone-tool-assisted consumption of animal tissues before 3.39 million years ago at Dikika, Ethiopia [evolutionary study; ungraded]
Journal of Human Evolution 2018: The manual pressures of stone tool behaviors and their implications for the evolution of the human hand [evolutionary study; ungraded] ↩
BioOne Complete 2014: An introduction to the isotopic studies of ancient human remains [evolutionary study; ungraded]
Journal of Human Evolution 2005: Isotopic evidence for diet and subsistence pattern of the Saint-Césaire I Neanderthal: review and use of a multi-source mixing model [evolutionary study; ungraded]
American Journal of Physical Anthropology 2006: Contributions of biogeochemistry to understanding hominin dietary ecology [evolutionary study; ungraded] ↩
Proceedings of the National Academy of Science (USA) 2009: Isotopic evidence for the diets of European Neanderthals and early modern humans [evolutionary study; ungraded] ↩
[hypothesis not based on clinical evidence article; ungraded] ↩
Journal of the American Medical Association 1929: The effect on human beings of a twelve months’ exclusive meat diet [case study; very weak evidence] ↩
Journal of Biological Chemistry 1930: Clinical Calorimetry: Prolonged meat diets with a study of kidney function and ketosis [case study; very weak evidence] ↩
International Journal of Tryptophan Research 2017: Meat intake and the dose of vitamin B3 – nicotinamide: cause of the causes of disease transitions, health divides, and health futures? [overview article; ungraded]
International Journal of Tryptophan Research 2017: Meat and nicotinamide: a causal role in human evolution, history, and demographics [overview article; ungraded] ↩
This is based on macronutrient grams. For example, if you were to eat 90 grams of protein in a day, you would pair it with 180 grams of fat. ↩
Crohn’s disease:
International Journal of Case Reports and Images 2016: Crohn’s disease successfully treated with the paleolithic ketogenic diet [case study; very weak evidence]
Type 1 diabetes:
International Journal of Case Reports and Images 2014: Type 1 diabetes mellitus successfully managed with the paleolithic ketogenic diet [case study; very weak evidence]
Reversing pre-cancer:
Journal of Cancer Research and Treatment 2018: Complete cessation of recurrent cervical intraepithelial neoplasia (CIN) by the paleolithic ketogenic diet: A case report [case study; very weak evidence]
Treating cancer:
J American Journal of Medical Case Reports 2016: Halted progression of soft palate cancer in a patient treated with the paleolithic ketogenic diet alone: A 20-months follow-up [case study; very weak evidence]
American Journal of Medical Case Reports 2017: Treatment of rectal cancer with the paleolithic ketogenic diet: A 24-months Follow-up [case study; very weak evidence] ↩
Clinical Review of Allergy and Immunology 2012: Leaky gut and autoimmune disease [overview article; ungraded] ↩
Gastroenterology 2020: Increased Intestinal Permeability Is Associated With Later Development of Crohn’s Disease [observational study, weak evidence]
F1000 Research 2020: All disease begins in the (leaky) gut: role of zonulin-mediated gut permeability in the pathogenesis of some chronic inflammatory diseases[overview article; ungraded]
Clinical and Translational Gastroenterology 2016: Human intestinal barrier function in health and disease [overview article; ungraded]
BioMed Central Gastroenterology 2014: Intestinal permeability – a new target for disease prevention and therapy [overview article; ungraded] ↩
Frontiers in Immunology 2017: Leaky gut as a danger signal for autoimmune diseases [overview article; ungraded] ↩
Patients ingest a standardized solution. If they have intestinal permeability, compounds in the solution cross the intestinal barrier and then are measured six hours later in the patient’s urine. The higher the level in the urine, the greater the intestinal permeability. ↩