Fasting and cholesterol

How can you lower cholesterol without medications? And what happens to your cholesterol if you do intermittent fasting?
High cholesterol is considered a treatable risk factor for cardiovascular diseases such as heart attacks and strokes. There are many nuances to cholesterol which I do not want to get into, but traditionally, the main division has been between Low Density Lipoprotein (LDL) or ‘bad’ cholesterol, and High Density Lipoprotein (HDL) or ‘good’ cholesterol — although those are grossly oversimplified.
We also measure triglycerides, a type of fat found in the blood. Fat is stored in fat cells as triglycerides, but also floats around freely in the body. For example, during fasting, triglycerides get broken down into free fatty acids and glycerol. Those free fatty acids are used for energy by most of the body. So triglycerides are a form of stored energy. Cholesterol is not. This substance is used in cellular repair (in cell walls) and also used for to make certain hormones.
The Framingham Heart studies of the early 1960s established that high blood cholesterol levels as well as high triglycerides are associated with heart disease. This association is much weaker than most people imagine, but results were slightly improved when LDL was considered separately from HDL. Since cholesterol is found at the site of atheromatous plaques, the blockages in the heart, it seemed intuitive that high blood levels plays a role in ‘clogging up the arteries’.
The question, therefore, became, what causes high blood levels of cholesterol? The first thought was that high dietary intake of cholesterol would lead to high blood levels. This was disproven decades ago. One might (mistakenly) think that decreasing dietary cholesterol may reduce blood cholesterol levels. However, 80% of the cholesterol in our blood is generated by the liver, so reducing dietary cholesterol is quite unsuccessful.
Studies going back to Ancel Key’s original Seven Country Studies show that how much cholesterol we eat has very little to do with how much cholesterol is in the blood. Whatever else he got wrong, he got this right – eating cholesterol does not raise blood cholesterol. Every single study done since the 1960s has shown this fact repeatedly. Eating more cholesterol does not raise blood levels.
So, if dietary cholesterol didn’t raise blood cholesterol, what did?
Low-fat diets and cholesterol
The next thought was that lowering dietary fat, especially saturated fats, may help lower cholesterol. Yet there is plenty of evidence to the contrary. In the 1960’s the Framingham Diet Study was set up to specifically look for a connection between dietary fat and blood cholesterol levels. This was the same Framingham as the famous Heart Studies, but references to the Framingham Diet study are virtually non-existent. Why haven’t you heard of it, before? Well, the findings of this study showed no correlation between dietary fat and cholesterol levels whatsoever. Because these results clashed with the prevailing ‘wisdom’ of the time, they were never published in a journal.
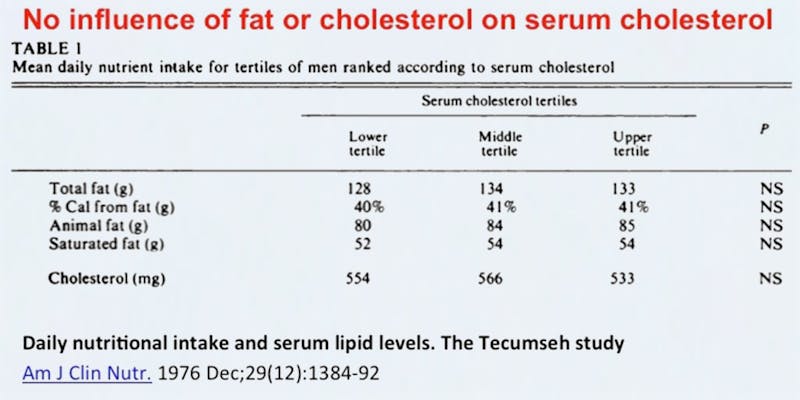
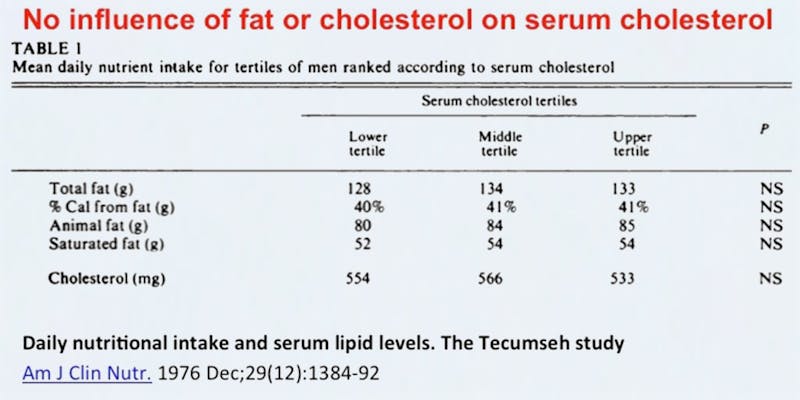
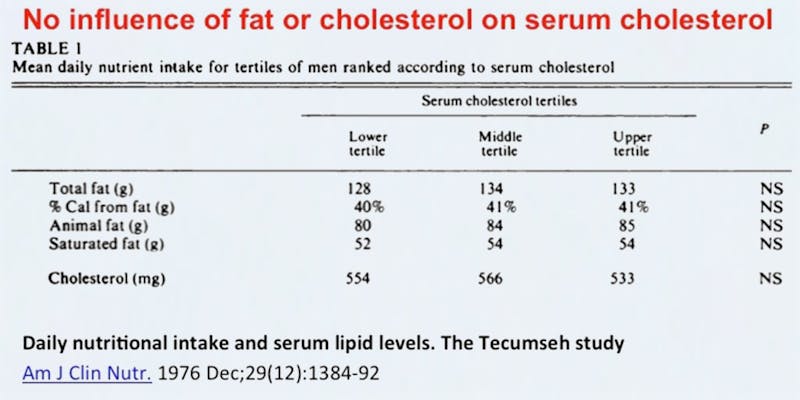
In some studies, extremely low-fat diets can lower the LDL slightly, but they also tend to lower the HDL so it is arguable whether overall health is improved. Other studies show no such lowering. For example, here’s a study in 1995, where 50 subjects were fed either a 22% or a 39% fat diet. Baseline cholesterol was 173 mg/dl. After 50 days of a low fat diet, it plummeted to… 173 mg/dl. Oh. High-fat diets don’t raise cholesterol much either. After 50 days of high fat diets, cholesterol increased marginally to 177 mg/dl.
Whenever somebody is told their cholesterol is high, they say “I don’t understand. I’ve cut out all fatty foods”. Well, reducing dietary fat will not automatically change your cholesterol. Some may see significant changes, but for most there are marginal changes at best. So, what to do?
“A little starvation can really do more for the average sick man than can the best medicines and the best doctors” – Mark Twain
Studies show that fasting is a simple dietary strategy that can significantly lower cholesterol levels.
Now, there are many controversies about lipids that I do not wish to get quagmired in. For example, there are many details about particle size and calculations of total particle numbers and newer particles etc. that are beyond the scope of this discussion. I will limit this discussion to the classic HDL/ LDL/ and triglycerides.
HDL
The lower the HDL, the higher the risk of CV disease. This association is actually much more powerful than that for LDL, so let’s start here. 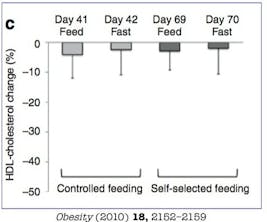
Several years ago, Pfizer poured billions of dollars into researching a drug called torcetrapib (a CETP inhibitor). This drug had the ability to significantly increase HDL levels. If low HDL caused heart attacks, then this drug could save lives. Pfizer was so sure of itself, it spent billions of dollars trying to prove the drug effective.
The studies were done. And the results were breathtaking. Breathtakingly bad, that is. The drug increased death rate by 25%. Several more drugs of the same class were tested and had similar effects. Just one more illustration of the ‘Correlation is not Causation’ truth.
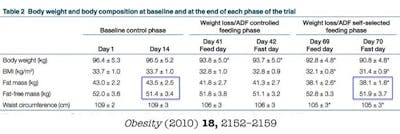
Nevertheless, we care about HDL because it is a marker of disease, just as a fever is often the visible sign of an underlying infection. If HDL is decreased, then it may be a clue that the underlying situation is also worsening. What happens to HDL during fasting? You can see from the graph that 70 days of alternate daily fasting had a minimal impact on HDL levels. There was some decrease in HDL but it was minimal.
Triglycerides
The story of triglycerides (TG) is similar, although there is likely more evidence that elevated triglycerides are more strongly associated with heart disease risk.
What happens to TG during fasting? There’s a 30% decrease in TG levels (good) during alternate daily fasting. In fact, triglyceride levels are quite sensitive to diet. But it is not reducing dietary fat or cholesterol that helps. Instead, reducing carbohydrates seems to be the main factor that reduces TG levels.
LDL
The LDL story is much more contentious. Statin drugs lower LDL cholesterol quite powerfully, and also reduce CV disease in high risk patients. But these drugs have other effects, often called the pleiotropic (affecting multiple systems) effects. For example, statins also reduce inflammation, as shown by the reduction in hsCRP, an inflammatory marker. So, is it the cholesterol lowering or the pleiotropic effects that are responsible for the benefits?
This is a good question to which I do not have an answer yet. The way to tell would be to lower LDL using another drug and see if there are similar CV benefits. The drug ezetimibe in the IMPROVE-IT trial also had some CV benefits, but they were extremely weak. To be fair, the LDL lowering was also quite modest.
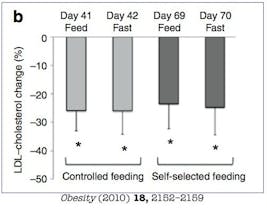
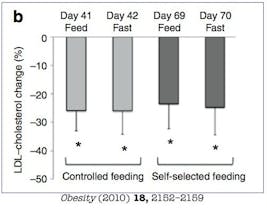
What happens to LDL levels during fasting? Well, they go down. A lot. Over the 70 days of alternate daily fasting, there was about a 25% reduction in LDL. To be sure, drugs can reduce them by about 50% or more, but this simple dietary measure has almost half the power of one of the most powerful classes of medications in use today.
But why does fasting work where regular diets fail? Simply put, during fasting, the body switches from burning sugar to burning fat for energy. Free fatty acids (FFA) are oxidized for energy and FFA synthesis is reduced (body is burning fat and not making it). The decrease in triacylglycerol synthesis results in a decrease in VLDL (Very Low Density Lipoprotein) secretion from the liver which results in lowered LDL.
One way to lower LDL is to make your body burn it off. The mistake of the low-fat diet is this – feeding your body sugar instead of fat does not make the body burn fat – it only makes it burn sugar. The mistake of the Low-Carb, High-Fat diet is this – giving your body lots of fat makes it burn fat, but it will burn what’s coming into the system (dietary fat). It won’t pull the fat out of the body.
Here’s the bottom line for those big-picture, spare-me-the-details kind of folks. Fasting has the following effects:
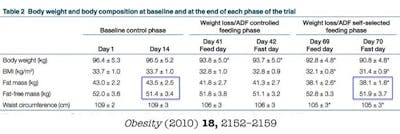
- Reduces weight
- Maintains lean mass
- Decreases waist size
- Minimal change in HDL
- Dramatic reductions in TG
- Dramatic reductions in LDL
That’s all good. Whether this will all translate into improved cardiac outcomes, I don’t have the answer for you. My guess is Yes.
That’s why I use fasting as a tool to help my patients improve their cardiovascular risk.
—
Jason Fung
More
Intermittent fasting for beginners
Popular videos about fasting
- MEMBERS ONLY
![The top 5 myths of fasting]()

- MEMBERS ONLY
![The 2 big lies of type 2 diabetes]()
- MEMBERS ONLY
![The cause of obesity]()
Earlier with Dr. Jason Fung
The Complete Guide to Fasting is finally available!
How does fasting affect your brain?
How to renew your body: Fasting and autophagy
Complications of diabetes – a disease affecting all organs
How much protein should you eat?
The common currency in our bodies is not calories – guess what it is?
More with Dr. Fung
His book The Obesity Code is available on Amazon.
His new book, The Complete Guide to Fasting is also available on Amazon.